It was a sunny July day eight years ago generic tadalafil. The first thing my hematologist asked me should have tipped me off: “Did you come alone?” The next four words he said will forever be etched into my memory: “You have multiple myeloma.”
Prior to my diagnosis, I’d been suffering from excruciating back pain, fatigue, and often felt myself forgetting things. This was beginning to impact my ability to effectively teach my fifth graders. I scheduled an appointment with an orthopedic doctor upon a colleague’s insistence. (In the past I just toughed things out without seeking medical help. I had never developed a relationship with any health care provider.) The orthopedist quickly diagnosed me with degenerative disc disease without ordering tests or imaging studies. My instincts told me to ask him, “How did you make the diagnosis of degenerative disc disease? Could it be anything else? Maybe we should do some imaging of my back?” But I grew up in the era of “Doctor Knows Best,” so I didn’t ask my questions and blindly accepted my doctor’s diagnosis.
For the next two years I was treated with various types of pain medication and physical therapy. Unfortunately, my pain didn’t improve. It actually was getting worse. Nothing seemed to relieve my distress. Not wanting to bother my doctor again (after all he already told me what was causing my agony) and thinking I had a low tolerance for pain I took matters into my own hands and managed to get through my day by consuming enormous amounts of over the counter pain medications. I should have returned to the orthopedist and insisted that he order more tests to discover the source of my extreme discomfort (or better yet I should have sought a second opinion). One day my colleagues found me sound asleep at my desk after I missed a scheduled faculty meeting. They insisted I return to the doctor, which I reluctantly did.
When I returned to my doctor and explained my fatigue and chronic pain he finally decided to take an x-ray. The x-ray revealed that several compression fractures in my spine were the source of my pain. I was scheduled for surgery to have the fractures repaired, but the surgery required medical clearance from my primary care physician, who in turn referred me to a hematologist when my blood work revealed I had severe anemia and a high sedimentation rate.
That’s how I ended up sitting across from a hematologist on a hot summer day, learning about my cancer. I had never heard of multiple myeloma so I thought it couldn’t be that bad. Boy, was I wrong. I didn’t really comprehend the seriousness of this diagnosis until after I went home and did some research.

Myeloma is a cancer of the plasma cells, which are a kind of white blood cell. Myeloma cells interfere with the production of all other types of blood cells, causing anemia, bruising, bleeding and recurrent infections. That’s why I was feeling so run down, out of breath and couldn’t get rid of that nagging cold. Also, the cancerous myeloma cells damage your bones. When I was shown an x-ray of my bones, they resembled Swiss cheese. They were filled with holes called lytic lesions. I also lost 3½ inches in height due to the compression fractures in my vertebrae. The degenerative disc disease that my orthopedic doctor had been treating me for over 2 years was really multiple myeloma.
I should have trusted my instincts and asked my doctor to take images of my aching back sooner. But back then I didn’t know that patients and doctors work together as a team. I thought I would be offending my doctor if I requested an x-ray since he was the one who had the medical degree. I didn’t think of educating myself about degenerative disc disease so I could have intelligent discussions with my doctor and ask questions about my treatment goals. My only discussions with my doctor revolved around my weekend plans, not my diagnosis.
Fighting myeloma has become the biggest battle of my life. My induction therapy stopped working after only a few cycles. I was extremely disappointed, but still very hopeful. My myeloma specialist recommended that I add a targeted therapy to my treatment protocol and proceed with a stem cell transplant, which I did. Unfortunately, the transplant did not have the outcome that we all anticipated. My entire team hoped I would be in complete remission after the stem cell transplant, but I only achieved a minimal response. I was devastated.
However, my myeloma specialist was hopeful and suggested different alternatives I could try. He gave me the pros and cons of each option and then offered his suggestion. Ultimately, it was my choice. It was at that point I realized that I was an integral part of my health care team and needed to educate myself so I could make informed decisions.
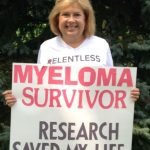
I am now an empowered team player. Patients who actively participate in their care experience better outcomes, fewer medical mistakes and are happier and healthier. Dr. Tom Ferguson coined the term “e-patient” before his untimely death in 2006 (from, ironically, multiple myeloma) as someone who is educated, equipped, empowered and engaged in their health and health care decisions. Meet e-Patient Cindy.
My metamorphosis from a passive bystander to an empowered partner on my health care team did not happen overnight. First I had to educate myself. The internet was my school and Facebook, Twitter, Smart Patients and countless podcasts and teleconferences were my teachers. Once empowered with knowledge, I had to practice speaking up and having my voice heard. I would challenge myself to engage in a meaningful discussion with my doctor at each consultation and to ask 2 questions. This was hard for me. It went against my upbringing, but I persevered. Practice made it easier and discussions became more natural. I am no longer the passive bystander blindly following doctor’s orders. I am an empowered partner. I feel confident in the decisions I need to make and I now encourage others to do the same.
Being an educator my entire life, it is only fitting that I use my passion for teaching to share what I have learned and continue to learn about the importance of patient engagement, myeloma resources, advocacy and myeloma research to a new group of students – patients, caregivers, doctors and anyone who will listen. My classroom no longer is the one story brick building on Pond Road, but the internet. I use various social media sites as my teaching tools. My personal Twitter handle is @MyelomaTeacher. I have close to 4,500 followers and tweet daily. Along with Dr. Michael Thompson, I organized the first #MMSM (multiple myeloma social media) Twitter chat and manage the @MMSMChats Twitter account. I am an administrator of the Philadelphia Multiple Myeloma Networking Group’s Facebook page and website. I also started my own Facebook page named Myeloma Teacher’s Multiple Myeloma Resource Page and have about 1,000 followers. Using Pinterest I created a series of myeloma-specific boards.
Myeloma CureTalks is an internet podcast talk show that features medical experts in conversation with a panel of patients about treatments under development. The person who was afraid to ask her orthopedist to take an x-ray of her aching back is now a regular panelist on this show asking myeloma specialists from around the world questions about their research. Additionally, I am on the advisory boards of the Patient Empowerment Network and the Myeloma Crowd Research Initiative and have presented at The American Society of Hematology (ASH) and the American Association for Cancer Research (AACR) annual meetings on the use of social media in patient engagement.
While attending the Mayo Clinic’s Social Media Residency as a patient scholar, I met Dave deBronkart (aka e-Patient Dave). He introduced me to the Society for Participatory Medicine. I immediately joined the society and have learned how important it is to own my data so I can make informed choices. I request copies of all test results and discs of all my imaging studies. I also ask for copies of my doctor’s notes and have enrolled in the patient portals offered by my various physicians. Remember that knowledge is power.
SPM also introduced me to Open Notes, a system in which patients and their designated caregivers can read every word their clinicians write, so they can be more informed. Unfortunately, I am not one of the 10 million patients who have access to Open Notes, but I am optimistic that that will change. As empowered patients, we are experts in our own disease and our own best advocates. To be able to make the best possible decisions we need to see ALL our data and for our health care provider to help us we need to fill in the blanks by adding to our medical record when we are experiencing something that may be related to our condition. Working together as a team is vital. I’m also learning how important it is to share my data with others. By sharing my data today I can be part of tomorrow’s cure.
Currently I am doing well. I have been in a very good partial remission for the last 3 years and continue to use maintenance therapy to maintain my remission. I am confident that if I should go out of remission I will be able to find another therapy to use. After all, four new therapies for multiple myeloma were approved in 2016! I keep up with all the new developments in myeloma and help others that need to seek new treatment options by providing them with sources to read and places to ask questions.
Change is possible. I have learned how important it is to be an active participant in your health care. You need to educate yourself, find support and have your voice heard. You need to own your data, understand your data, add to your data, use your data to make informed decisions and share your data with others.

