The Society for Participatory Medicine, through its founders and mission, has a strong belief in the expertise of its patient members – many of whom identify as providers or journalists or have expertise in HIT, health economics and other areas.
Patients, often through the marriage of acquired experience and the skills they bring with them into patienthood, have a vast amount of expertise. It turns out, these expert patients have already considered solutions to many of the challenges hospitals and health systems are currently tackling. The wonderful thing about these solutions is they are inherently patient-centered design. We’ll be sharing these patient-designed solutions via this site.
In a recent blog post, healthcare process and quality improvement champion Paul Levy quotes Rob Markey. Markey, whoes content appears on the HBR Blog Network writes about how to learn nothing from patients:
If I were writing a “how-not-to” manual for customer feedback — a manual that would guarantee your feedback system taught your employees nothing about how to delight customers and earn their loyalty — here are the five rules it might include:
- Aggregate the feedback into scores, percentages, and averages — and stop there.
- Hold the feedback.
- Eliminate the human voice.
- Ensure that there’s a lot at stake.
- Never close the loop with customers.
Great minds, as they say, think alike. Around the same time, SPM members were having a discussion around a similar topic in the membership email group:
What 3 things could hospitals do to be more participatory?
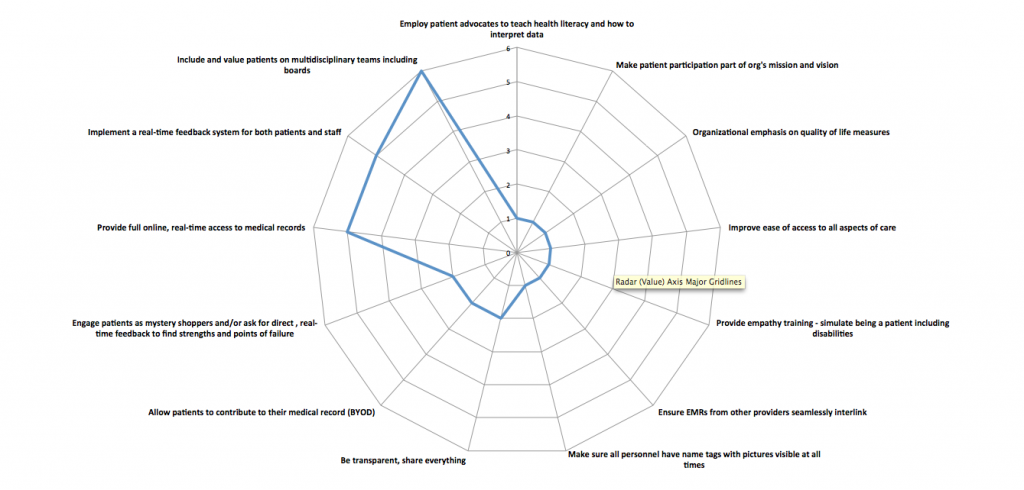
Over 20 members weighed in with their own top three suggestions. I have categorized those answers and grouped them accordingly. Here are the results, presented as a spider graph:
note: the further an item is towards the outside of the web, the higher number of votes it received.
The top three suggestions, as defined by expert patients, are:
- Include and value patients on multidisciplinary teams
- Implement a real-time feedback system for both patients and staff
- Provide full online, real-time access to medical records
What makes this list so great, in addition to being created by patients? The top three suggestions are all doable and they are doable now, with few or no new resources required.
Hospitals can immediately begin including patients on committees, strategy teams, and advisory groups. Providers can involve patients in their own care and treatment planning. It doesn’t take much more than a Twitter account and Facebook page to invite real time feedback. But for the organizations interested, there are startups specializing in providing real time feedback platforms for hospitals. And, finally, meaningful use compliance is moving us towards a world where real-time, complete record access is required; wouldn’t it be nice to be ahead of that curve?
Participatory is about co-design — strategies, processes and services co-created with patients who are equal members of the team. We will, from time to time, continue to publish insights from our membership’s expertise. If there is a challenge for which you like the Society’s member’s insight, leave a note in the comments.






Big yes and “of course” to including patients on multidisciplinary teams but/and a key variable to take into account: for how long has the patient has been diagnosed and undergone (or opted out of) treatment.
Having lived with a chronic illness for nearly 30 years, I’ve seen my own ability to communicate about it more clearly and constructively emerge over time.
Please don’t get me wrong, I can still work up a lot of disgust with the healthcare system (and especially Big Pharma), especially if I’m in physical pain, but I’m simply not as outraged as I was for the first five to eight to ten years. For example, my perceptions about and attitudes toward medical practitioners has changed in fairly significant ways.
My point? In addition to many other variables, patient input will be shaped by how long the patient has lived with her/his condition/disease. I say this needs to be factored in when inviting participation.
Meredith,
I absolutely love your comment. You are reminding us that patienthood is multidimensional. It’s not linear. A number of factors make up the matrix of someone’s journey including length of time living with a given condition.
We should also take into account the severity of impact a condition has one one’s life, the number of simultaneous health issues someone is dealing with, their resources (including socioeconomic and caregivers), etc.
In short, shouldn’t we view and value people as the whole person, and not just their health condition(s)?
And even more to be explored and discussed: What does it mean to be an “epatient”? When do people opt-in or out of that self-identification?
Relative to the whole person: Is it time (especially given what we know about SBNR [spiritual but not religious] types) to have conversations about the spiritual dimension(s) of health and identity early on?
Clearly I have a lot on my mind these days!
Great Post. Thanks for Sharing…..