Preface by e-Patient Dave: We have often written here (see posts) about Shared Decision Making, in which patients are engaged in choosing among treatment options. A key method is to give patients a “decision aid” (DA) – a document or video that explains the options, with pro’s and cons.
A vital question in the design of a DA is, which factors should patients be informed about? And who decides that? In this case a researcher is asking for patient opinions (!) on what should be included in a DA for stents. (See the National Institutes of Health introduction to stents.) SPM member Marilyn Mann (@MarilynMann) knows a lot about stents – this is her first post here.
Adnan Chhatriwalla, MD, is a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, and is co-investigator for DECIDE-PCI, a study designed to develop and test a decision aid (DA) for patients who have decided to have one or more stents inserted in their coronary arteries. (Note: this is not about whether to have a stent at all — that would be a separate decision.)
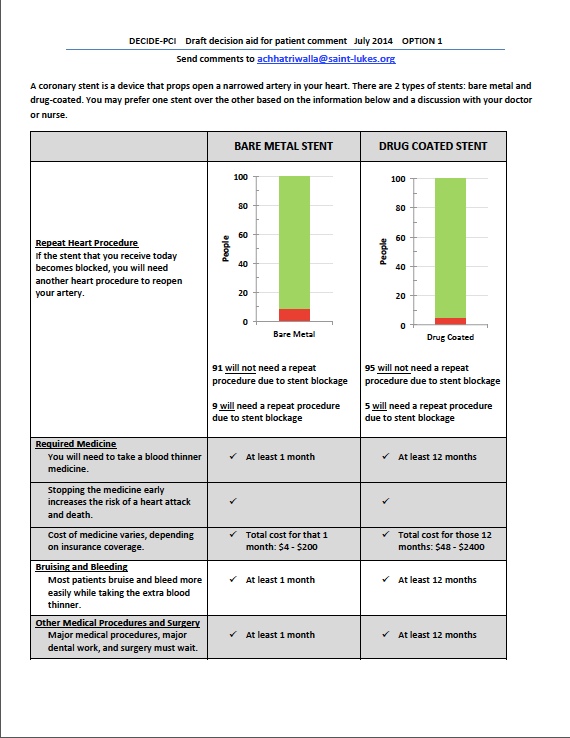
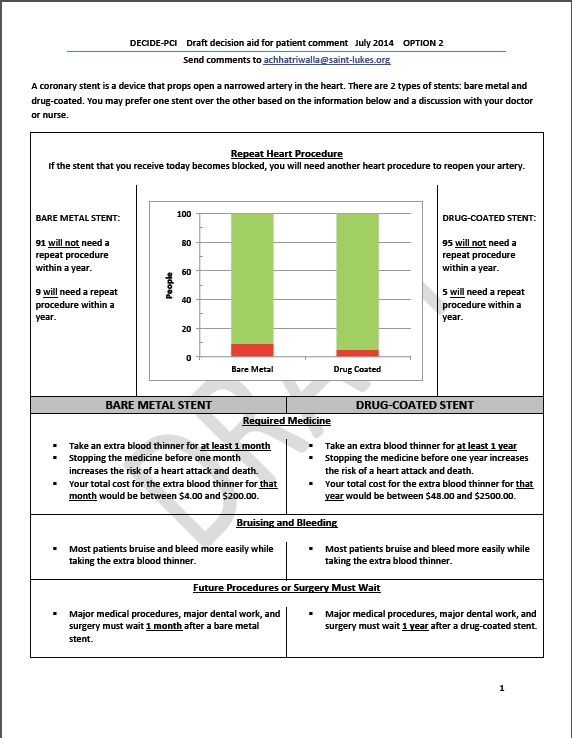
The DA would help these patients choose between the two types of stents — bare metal stents and drug-eluting stents.
One of the drawbacks associated with stents is that over time, scar tissue can grow into the artery and make it narrow again. This can make it necessary to do another stenting procedure to open up the artery. “Drug-eluting” stents are coated with drugs that reduce the risk of the scar tissue forming and narrowing the artery. However, drug-eluting stents have the drawback that they require the patient to take blood thinners for a much longer period of time, as compared to bare metal stents. This adds costs and increases the risk of bleeding.
The study is in the beginning phase, and the researchers are engaging patients in focus groups to better understand what factors are most important to them in choosing a stent. The focus groups will also involve asking patients how they prefer the information to be presented (e.g., in words, graphs, some combination of the two, and so forth). Later, the decision aid will be tested at two hospitals to see if it improves patient understanding and satisfaction, and if the use of the decision aid changes the percentages of bare metal stents and drug-eluting stents received by the patients.
Dr. Chhatriwalla is very interested in getting feedback from patients and others on the current drafts of the decision aid (two different versions) and has asked SPM to help circulate them. You do not need to be a heart disease patient to participate — the researchers are interested in a wide range of viewpoints. Please take a look at both of them (posted below) and send your comments to Dr. Chhatriwalla at achhatriwalla@saint-lukes.org.






Great tool and thanks for asking us at SPM to weigh in on this!
In the world of higher deductibles, I think it is essential to give us an idea of the overall costs for each option: the device, surgery, hospitalization, physicians. Are the costs identical?
Also it’s not clear to me what the second procedure would entail: the same thing as before (double the costs) or some other procedure?
In terms of layout, I like the first version where the comparisons are closer together.
Agree with Ileana completely — about everything!
Want to underscore that Option 1 is much easier to read. Minor design tweak: Remove underliningunder whatever is bold to enhance readability.
I find both quite readable, but am alarmed that the patient may think that the requirement to use blood thinners would preclude ANY surgery. I do assume that if another health problem arose in which surgery is needed, that going off the blood thinners for a period of time would be recommended and without a big increase in risk. That should be explained, as that may preclude a fully informed choice.
One important missing piece regards the ramifications if surgery of some sortshould become required, due to accident or emergency, within the exclusion period post-implant. I prefer layout #2. And, the checkmarks in #1 are at best meaningless and at worst seem to imply something…
Ditto on including total procedure costs.
How about something regarding potential complications?
Bart, YES! Complications and side effects with risks attached.
LOVE this! Prefer Option 1, bc it is visually more intuitive. Miss info on what drug that stent is coated with, its possible side effects and what will happen if I experience these side effects once the stent is in my body (ie. will it be removed). Also lacking info on cost of one stent vs. the other?
Comments that apply to both versions:
1. “Repeat heart procedure” is not self-explanatory. Most patients do not understand what a cardiologist means by a “procedure” or “surgery,” or what the difference is between those terms. Would the consequence of stent blockage always be insertion of another stent? If so, perhaps “repeat stent procedure” would work.
2. You need to indicate that the numbers are out of 100 people. Also suggest putting percentages in parentheses.
3. The meaning of green and red in the figure is not explained. Suggest that the relevant numbers be shown in red or green, as applicable.
4. Suggest a more explanatory label on the Y axis (e.g., “Number of people per 100 who will (red) or will not (green) need a repeat stent procedure”).
5. I wonder if there is anything beyond one year that the patient should know?
6. With respect to bleeding, how often would this result in hospitalization and serious complications?
7. Agree with the commenters who stated that it is not clear what would happen in the case of an emergency requiring surgery.
Comments on Option 1
1. You need to state the time period (i.e., one year).
2. Suggest deleting all the check marks and inserting “Yes” in the boxes for stopping the medicine early.
3. The meaning of “blood thinner medicine” is not clear. The patient needs to know that they will need to take aspirin for the rest of their life plus an extra blood thinner such a Plavix for the required period.
Comments on option 2
1. The meaning of “extra blood thinner” will not be clear to most people. You need to state that aspirin will be required indefinitely in both cases, plus an extra blood thinner such as Plavix for the required period.
General impression: I found Option 2 much easier to read and digest.
I am not sure the figure works that well. To me, the important thing to know would be the percentage of people who need repeat procedures. I suggest testing a version of the figure that only shows that information. You could still have the number of people who don’t need a repeat procedure explained in the text.
Marilynn, are these comments that you sent to Dr. C?
Well, I sent him an email telling him that I had written my comments here.
Okay, because I want to be clear (for all readers) that his instructions (in the post!) were to write to him directly.
Of course people are welcome to post here – as you noted, he’s reading here – but nobody’s required to, if they’d rather be private in their feedback.
Thanks!
Thanks everybody for your feedback, this is so valuable to us. We have been looking at these posts but I have received emails as well, and either is fine.
For the record, here I’ll paste in my own notes on Option 2, which I sent to Dr. Chhatriwalla before we did this post.
__________
I had several immediate reactions:
– The blog post says “eluting” and the DA says “coated” – as you know, I much prefer the latter for clarity.
– “The stent you receive today…” Today?? Is this intended to be used right before a procedure, with no time to consider at home?? I don’t think that’s either wise or courteous to the patient. Why not remove “today”?
– “Need a repeat procedure” is way less clear than necessary. Why not say “need to have the stent replaced” or “need another stent operation”?
– The facts presented on the page are clear enough, but it would be great to have a concise orienting introduction, e.g.: “There are two things to consider: the chance you’ll need another stent within a year (drug-coated is better), and how long you’ll need medication after the surgery (bare metal is better). The choice is up to you.”
– Finally, there’s one BIG patient-oriented factor not in the DA that I’d want to know: Is there any difference in survival or MI recurrence between the two?? Frankly I’d put that at the top, ahead of whether another stent will be needed.
I know in general that stents don’t reduce recurrence, but if it were me I’d still ask if the data in those studies showed any difference [between the two options in this DA].