(part three of three)
Lessons from Quebec for Choosing Wisely and Less is More Medicine
After a busy few days tracking topics around the researchers and policy-makers at a recent “Preventing Overdiagnosis” conference in Quebec aimed at reducing over-treatment in modern medicine, I came away with the impression of an evolving ecosystem. The Choosing Wisely campaign and their allies in the ‘Less is More’ cohort (also known as ‘minimal medcine’), have been been consistently gaining steam for reducing waste, error and over-treatment, but the movement is still transitioning, still testing, and still thinking about how the patient fits in.
 Victor Montori MD of Mayo (“Minimally Disruptive Medicine“) caught one sense of it when he wrote “The Answer is Not In” as the sub-title of his journal piece about shared decision making (#SDM). He feels we don’t yet have enough long-term statistics to make a solid claim about how much SDM helps improve the outcomes or the experience.
Victor Montori MD of Mayo (“Minimally Disruptive Medicine“) caught one sense of it when he wrote “The Answer is Not In” as the sub-title of his journal piece about shared decision making (#SDM). He feels we don’t yet have enough long-term statistics to make a solid claim about how much SDM helps improve the outcomes or the experience.
In a parallel lane aimed at less, but more effective, medicine, Dr. Vinay Prasad of Oregon, a vocal advocate of what is sometimes called “de-prescribing,” notes it is already clear that “many current medical practices have no convincing proof of efficacy” and he drives home the point in this journal piece An Analysis of 146 Contradicted Medical Practices.
Multiple speakers also shared useful lists of practical points from the front lines, including the sum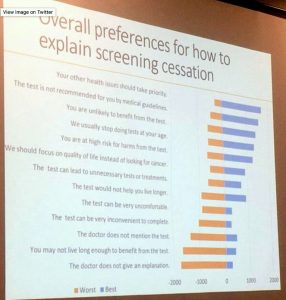 mary at right, describing patient preferences on the topic of excess testing which adds expense but little medical benefit (click image to enlarge and read). I was especially pleased to see the focus of the query, reporting on what patients said were the most reassuring or helpful reasons given to explain why some tests have been used to excess. (See also the end of this post for more about the multiple things “patient-centric” can mean .)
mary at right, describing patient preferences on the topic of excess testing which adds expense but little medical benefit (click image to enlarge and read). I was especially pleased to see the focus of the query, reporting on what patients said were the most reassuring or helpful reasons given to explain why some tests have been used to excess. (See also the end of this post for more about the multiple things “patient-centric” can mean .)
The BMJ also assembled a very useful list when it published this detailed analysis of the “drivers” of excess care. The article began by looking back at the origins of the problem:
“In our collective enthusiasm to diagnose and treat disease, a growing body of evidence indicates that we may often be doing too much of a good thing. “Overdiagnosis” is now widely recognized to occur when people are labelled with or treated for a disease that would never cause them harm—often as a result of undergoing screening—and it can lead to the overuse of further tests and treatments. One example is thyroid cancer, with estimates that over 500 000 people may have received overdiagnoses across 12 countries in the past two decades, leading to unnecessary surgery and lifelong medication for many. Overdiagnosis is a challenge to the sustainability of human health and health systems. Its causes—including the best of intentions—are as complex and multifaceted as the potential solutions..”
Mapping the drivers of overdiagnosis to potential solutions
BMJ 2017; 358 doi: https://doi.org/10.1136/bmj.j3879 (Published 16 August 2017)
Cite as: BMJ 2017;358:j3879
The article charted many obstacles and tied them to many antidotes. Paraphrasing from their charts to my own summary below, the factors that set us up for excess and unneeded treatment include:
- Culture
causes: habit, tradition, outmoded beliefs such as ‘more is better’, biased media coverage, over-medicalization of maladies
antidotes: awareness campaigns (public, professional), attitude shift (healthy skepticism), higher tolerance for uncertainty, better press - Healthcare System Issues
causes: financial incentives, too many silos between groups, pressure to produce good statistics, screening ahead of symptoms, inflexible use of guidelines, tests that are too sensitive, complexity of care and lack of coordination
antidotes: convert incentives from quantity to quality, reform definition of diseases, more research statistics about overtreatment (#otx) - Clinician Customs and Concerns
causes: fear of litigation, fear of missing an illness or injury, spotty training, lack of confidence or knowledge, over-reliance on tests
antidotes: shared decison-making (#SDM), tort reform (especially in the U.S.), education cmpaigns (public and pro)
All in all, this article gave a very effective road map for steady incremental development. Is it the kind of cause this is likely to go viral or kindle virtual armies of activist patients? I doubt it, for reasons going back to “Occupy Health” and before. So many have tried to spark a mass movement, and none have managed it yet. In a future post or few, I hope to explore some of the reasons why this might always hold true.
Subject, Object, Cart and Horse:
The Multiple Meanings of ‘Patient-Centric’
The cartoon above was also plucked from the social media stream around the conference in Quebec. It is cute on its literal face (a patient diametrically centered between two clinicians ignoring each other while focusing on their computers). But it could also be a joke about the lip service sometimes paid these days to putting the patient front and center.
I found that out the hard way early this decade when I had a chance to be part of the first patient cohort attached to a group of clinicians who were vetting grant applications. I applied thinking it was a chance to give input to people who wanted to be more responsive to what patients seek, or to what they feel is lacking. Instead, once embedded, I found out the goal was about how to get patients to comply with what the study designers wished them to do. Increasing compliance by patients was the aim, not increasing compassion or convenience provided to them.
Quite a reversal of cart and horse.
As it turned out, a similar sort of miscue often applied to the early years of research based on “patient outcomes.” The experience or opinions of patients was irrelevant. They were objects to be measured, weighed, surveyed and counted on the way to obtaining statistics to serve as evidence. Don’t get me wrong, the early days of evidence-based (#EBM) medicine last decade were essential to the shift we have made this decade to asking what worked or did not, and those statistics are what enabled us to see the whole problem of overtreatment.
My point is you should not assume simply because you see a term such as “patient-centric” or “patient focused.” You need to ask who is being engaged in which ways to what ends before you decide how — or if — the needs of the patient are being served.






Recent Comments