I don’t get surprised these days as easily as I used to before I got “e.” But something popped my eyes open last weekend, and I dug into it. It goes to the heart of where the power is, in the doctor-patient relationship. But not just the power – the responsibility for getting it right. Yikes.
A new book, Patient, Heal Thyself, is reviewed in the 12/26/08 New England Journal of Medicine (review here; subscription required). I’m a bit stunned by author Robert Veatch’s apparent position on “patient autonomy,” but I soon learned that his utopian-sounding views may be closer to reality than I imagined.
Still, it seems a bit much. Reviewer Mark Hall, J.D., of Wake Forest, says:
Veatch’s proposals are so startling that readers of this review may doubt my characterizations, so I will quote liberally, starting with its excellent title — Patient, Heal Thyself. This injunction captures Veatch’s two main points: Patients alone are in charge, and they have no choice but to assume this active role. According to this “manifesto,” doctors “will no longer be seen as capable of determining what will benefit their patients. It is patients themselves who, in the world of the new medicine, have to take charge.”
As someone whose butt was saved by excellent medical care, I find it unimaginable to consider doctors “incapable of determining what will benefit” me. What, like I was going to think up high-dosage Interleukin-2 on my own?
But whether we accept every word in the book (which I haven’t yet read), let’s step back and look at those two main points.
Patients alone are in charge: Working group colleague Charlie Smith MD wrote about the review, too. He reminds me that patients are indeed in charge of what gets done; a major concern doctors discuss all the time is compliance: whether we slacker patients will actually take the recommended medication (I do), heed dietary recommendations (oops), get checkups at recommended intervals (mezza-mezz), etc.
And I realized, it goes beyond that: a friend of my family developed kidney cancer a year after I did, and elected not to get treatment where I did – he stayed with his local hospital (also in the Boston area), and is dead now. Who was in charge? Clearly he was. And that leads to the second assertion:
[Patients] have no choice but to assume this active role. A vital question is whether the patient realizes this – or, more to the point, realizes the implications. Did our friend fully comprehend the implications of his choice? Was he “e”? Was he empowered or hopeless? Talking to him, I was never sure, but it didn’t feel like he felt he could influence the outcome.
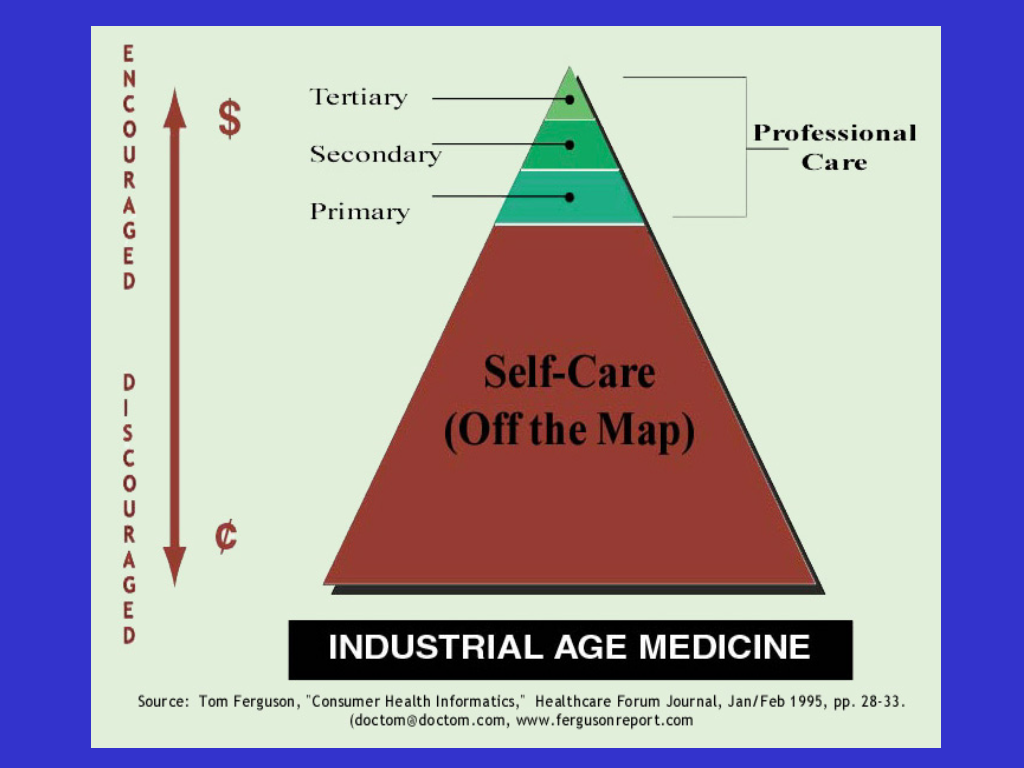
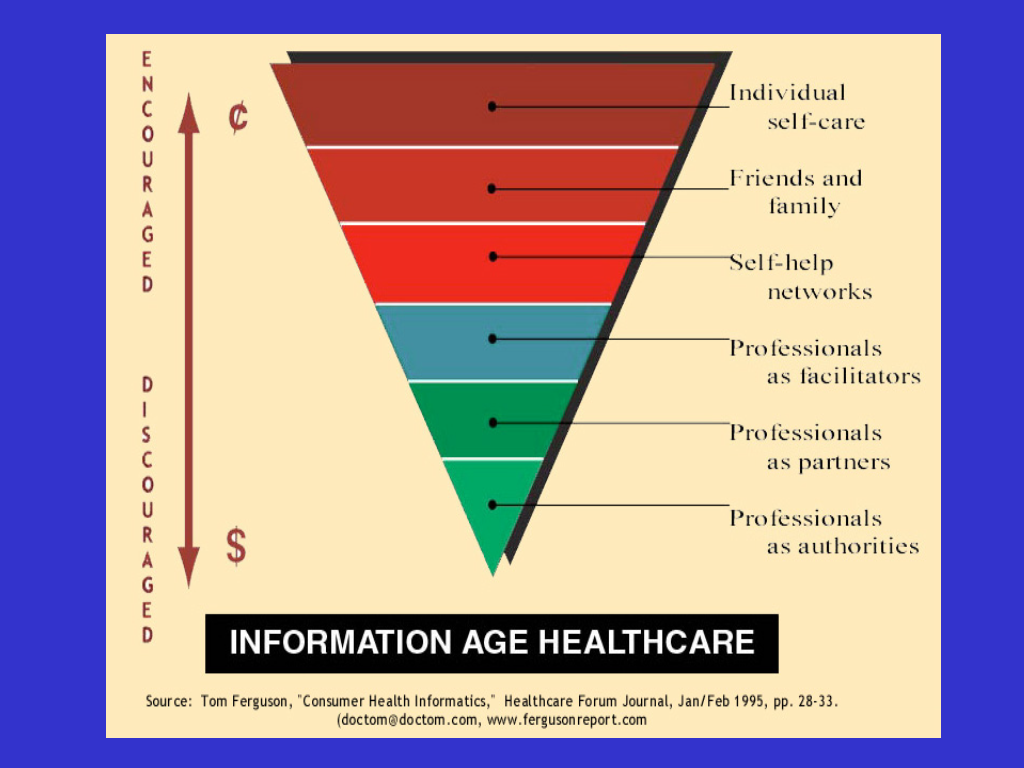 But then I thought back to “Doc Tom” Ferguson’s visionary slides, dating back to 1995, predicting that patient access to medical knowledge would turn healthcare on its head. (Click to enlarge.)
But then I thought back to “Doc Tom” Ferguson’s visionary slides, dating back to 1995, predicting that patient access to medical knowledge would turn healthcare on its head. (Click to enlarge.)
The vast majority of tough thinking and wonk work on blogs like THCB, and at conferences, is about the ugly tangled mess American healthcare has become. I’m not belittling that work – it needs to be un-messed – but while that work continues (and regardless of its progress), the real juice for each patient now, today is in how well we take responsibility for our care, by informing ourselves and making choices.
Charlie nailed it in the close to his post: “What lessons does Mr. Veatch’s book leave with us? …It is a good wake up call for physicians. We need to embrace the ‘ePatient Revolution’, recognize that the patient MUST be the one who is in control of their own health care, assist them in achieving this, and not be tempted to allow that to interfere with our professional self esteem because, in my view, it in no way threatens it!”
That echos last week’s post “Physicians are coaches, patients are players.”
Or, as my primary physician Danny Sands put it when he and I spoke at Connected Health in October:
- Embrace knowledge symmetry.
That’s the core of it. See our banner graphic – “health professionals can’t do it alone.” We the patients do need to accept that not only do we have the right to guide our care, doctors need our help – and we need their guidance.






I just ran across one of my first posts ever on this blog, When the Patient is a Yahoo. It was on a different subject but it ended up in a similar place.
It’s increasingly clear that the unifying thread in this movement is partnership, collaboration, what we’re calling participatory medicine.
Nice article with insights of patient & physician relation.
Dave,
Wonderful post, and I greatly appreciate both you and Charlie Smith writing about this book/review. These ideas can not get enough attention, (and I mean that in a less positive way than you think).
I suspect that I”m pretty much an average doc, not the smartest, not the dullest. BUT, one thing I somehow understood better than my colleagues at an early stage in my career was that I can not know everything. I can only try to find the best guidance for my patients, and to present it to them in a way that they can understand. That leaves pretty much everything else up to them.
But as your own run down of your “adherence” to what you know to be important demonstrates, we all make choices as patients that are not in our best interests. Chances are, a lot of people reading this post are overweight, some smoke, many drink more than is healthy. Almost none get enough exercise, and definitely get too little sunlight/vit D. In my own sub specialty, the vast majority of my patients with poorly controlled epilepsy drive, when I’ve pointed out that state law says they must turn in their licenses. Many miss medications regularly, do not get enough sleep, and lie to their employer about their condition.
Recently, the Supreme Judicial Court in Massachusetts LOWERED the bar for holding practitioners responsible for lots of this behavior. When I’ve held focus groups of my patients, not just my e-patients, I find that the former make up the vast majority of my panel, and they are NOT INTERESTED in taking an active role in their care. They do not want to use the same technologies with providers that they use with friends and even retail business.
Many providers who have embraced e-patients find it much more fun and rewarding, but there are not enough of them. A friend decided he’s only take on patients who are e-patients and found that he had a tiny, concierge practice. So, please, by all means write on this topic, shout it from every hill if you have to.
The possible meanings of patients “taking charge” are varied and deserve some attention:
1. “OK, go ahead, take charge” (if you think you can, and Internet sources can supplant physician expertise) (*no patient can match the expertise of a physician, nor can any Internet source). This seems like a deliberate misunderstanding of PM.
2. take charge because the health care system is broken; you have no choice. This is practically true where I live, and for my demographic;
3. go ahead, take charge, it absolves us of legal liability
The best meaning is “take charge, enter into a fully responsible and educated partnership with your physician; see what we can accomplish together.”
There is a flip side to participatory medicine, reflected in physicians’ dominant view of patients. “I am tired of doing so much for your health, when you do so little.”
This must necessarily be a valid part of PM:
Implied and stated here is a Call to Patients to Step Up: If you want your physician’s respect, if you want to be healthy rather than assured that you are “ok” when you are not, YOU, the PATIENT, has to change, too.
Docs on The Health Care Blog are bitter about sharing records with patients because 1) there is no profit in it; and 2) their experience of patients (which they perpetuate through their own Dr. Knows All protocol) is that patients are passive, uneducated and self indulgent.
As a teacher, I often feel the same way: Why should I put more energy into a student than the student or family does themselves?
The good news: From my end, I can encourage a new generation of students to invest in literacy in order to save their own lives and those of their loved ones. Here, they will have no choice. The American health care system is broken and will not be fixed in the near future. In our area, which has a dearth of specialists as well as pcps, if you don’t get educated, you can die.
Participatory Medicine means that BOTH SIDES CHANGE. I teach in a distressed economic area where kids’ main snacks at school remain Cheetos & Coke, despite all of the health care warnings plastered everywhere (at taxpayer expense) about the risks of childhood obesity.
GOOD COMMUNICATION IS GOOD MEDICINE
One solution is for physicians to come out from behind the professional aura of Rational, Emotionless Scientist. Find a site to Express frustrations in a way that their patients can HEAR. Instead, patients often get the body language, the curt attitude, etc. that implies rather than states that they are less than nothing and the unspoken thought: “Why should I hand over test reports if you are too lazy or uneducated to decipher them on your own? Take the pill and leave.”
WOW!! Was I sleeping when you all wrote these comments?? Great blog and great comments. I agree wholeheartedly – good communication = good medicine; let’s have knowledge symmetry (and I would argue also for knowledge diversity); let’s move medicine away from its scientist face or at least bring its human face back into the picture and the golden rule of collaboration. Moreover I would argue, based in relationship centered care that this communication, knowledge symmetry, collaboration and human face should extend beyond the patient-provider relationship to the peer relationships and the relationships everyone has in their community. That is where the e-patient will take us in the end, to a community of knowers and hopefully, agents for better health and better care! Bravo to you all! Now if we could just feed that message back into med schools……..