Through the magic of Google Alerts, Diane Engelman recently learned of this blog. She’s one heck of an e-patient, though until now she’d never heard the word.
That proves patient empowerment is a real trend, driven by a powerful force: the desire to help oneself – or, often, one’s child – in any way possible, using every possible resource, which today includes the internet and social connections. (Yes, real medical value from connecting with non-MDs.)
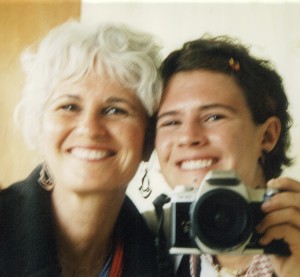 In this case a large health plan was out-thought, outresearched and outmaneuvered by one of the most potent e-patient subtypes: the “Mama Lion.” The plan’s own cardiologists unanimously said Diane’s daughter Hilary needed mitral valve surgery, but the staff surgeons repeatedly said no – largely because, one suspects, they didn’t have adequate expertise for the appropriate surgery and didn’t want to pay to have it done out of network.
In this case a large health plan was out-thought, outresearched and outmaneuvered by one of the most potent e-patient subtypes: the “Mama Lion.” The plan’s own cardiologists unanimously said Diane’s daughter Hilary needed mitral valve surgery, but the staff surgeons repeatedly said no – largely because, one suspects, they didn’t have adequate expertise for the appropriate surgery and didn’t want to pay to have it done out of network.
Instead they urged Hilary to hurry up and have babies while she could, wait excessively long for necessary surgery, and accept their claim that they were adequately qualified to do it when they clearly were not.
This is a long, true, inspiring story of an empowered patient/family using the internet to drastically alter the outcome for the better. She’s had this story written for a year and has been looking for a place to publish it. So glad you found us, Diane – and mazel tov, Hilary!
Through the Land of Oz:
Self-Advocacy in Today’s Health Care System
by Diane H. Engelman and JB Allyn
In January 2003, the cardiologist declared, “You should have your babies right away. Your heart valve will need replacement and it will be difficult, maybe impossible, to have kids after your operation. You have the choice of a pig valve or a mechanical valve.” My daughter, Hilary Engelman, was 23 years old, not married, and not yet thinking of having children. After the cardiologist’s pronouncement, we cried, not for the only time on this medical odyssey.
Hilary had been diagnosed at age seven with mitral valve prolapse (MVP). Since she had no symptoms, doctors relied on echocardiograms – sound waves that create a moving picture of the heart – to give an accurate, quick assessment of her overall heart function. Initially, they thought her condition was a benign heart murmur, the case for many people with prolapsed mitral valves. Three years after first diagnosis, though, a pediatric cardiologist at our health maintenance organization (HMO) said, “Your daughter’s MVP is not trivial and may require surgery someday.” With a hint of sadness in his voice, he pointed to a photograph of a vibrant-looking teenager on his bulletin board and added, “A patient of mine died from a leaky valve like hers.”
I had been a member of this HMO since before Hilary’s birth. Both my children were born there and we had received great care. I trusted them to follow her condition vigilantly, but this physician’s deadly comparison irritated me. It also got my attention and started us on our long journey toward understanding the exact nature of her heart valve problem and how to fix it. I did what any mother, any consumer can do – I stubbornly sought every piece of information available on MVP. For three days following that appointment I read and cried, cried and read, relieved to uncover facts but fearful for the future.
I found that the medical phrase “mitral valve prolapse” referred to a condition more than a diagnosis, describing a range of heart valve variation, from benign to malignant. The mitral valve controls blood flow between the upper and lower chambers in the left side of the heart. Blood should flow only one direction, from the upper chamber into the lower. If these valve flaps do not work properly, part of the valve may “balloon” into the upper chamber and regurgitate, or leak.
Over the years, doctors applied a dozen descriptors to Hilary’s malfunctioning heart valve, including deformed, flailing, floppy, and, her least favorite, ugly. For consumers like us, this list did not cast more light on her condition. We knew only that her valve was “prolapsed,” and a prolapsing valve does not necessarily mean anything medically important. Many people walk around with prolapsed mitral valves and never need treatment, much less open-heart surgery.
Cardiologists, who treat disorders of the heart that can be managed non-surgically, followed my daughter’s case over the years. With no symptoms and semiannual passable echocardiograms, we slipped into a shared, dangerous illusion of good health. But with the 2003 warning that Hilary should have her babies right away, surgery suddenly hung over us again. I arranged for several surgical opinions, and during this round of consultations, a cardiac surgeon first uttered the dreaded words, “Your daughter’s valve is probably not repairable.” But at the time, cardiologists and cardiovascular surgeons said she did not need an operation, at least not yet.
Then, in December 2007, two HMO cardiologists warned that surgery should happen within a month. Although we had long expected this day, its arrival overwhelmed us. Hilary said to one doctor, “You have no idea how hard it is agreeing to surgery when I have no symptoms. I feel fine!”
Compared with her echocardiogram from six months earlier, her valve now leaked severely, creating two jets – an ominous finding. Blood pressure increased in the arteries supplying her lungs, and her heart muscle showed signs of exhaustion. If leakage forces the heart to work too hard to pump blood, its function will eventually decline. Damage to a heart muscle is irreparable and permanent. Her primary cardiologist warned that shortness of breath, dizziness, and fainting on exertion were not far away and immediately referred her to our HMO’s cardiovascular surgery department to schedule a heart operation.
Her heart murmur had turned out to be more than a variant of normal. It was on the severe end of the MVP spectrum, and, uncorrected, a valve like hers may lead to a heart transplant or even death. Hard enough to think she would require open-heart surgery, but knowing she had the kind of valve that her doctors considered too difficult to repair left us numb.
Clinging to the life raft of current literature, most of it available on the Internet, I discovered critical information. Her defective valve might actually have a name: “Barlow’s valve,” a consequence of “Barlow’s disease,” first written of in the 1960s. None of the HMO physicians had mentioned this label, though it fit uncomfortably well with their many descriptions of her troubled valve. I was relieved to find a possible diagnosis, hoping that a specific label for her valve might also mean a specific treatment.
Second, I found that the likelihood of successful childbirth lowers after mitral valve replacement. When I initially understood that my daughter’s heart condition might require surgery, a friend, a cardiac-nurse specialist, had mentioned that mitral valve repair, not replacement, was the best surgical treatment. She said that too many patients with severely-leaking heart valves receive replacement valves instead of repairs. With mitral valve repair superior to replacement, the choice between the two matters to all patients and is a crucial detail for a woman, such as Hilary, who is yet to have her children.
Third, and perhaps most significantly, I discovered why physicians had not given Hilary’s prolapsed mitral valve a more specific label. The reason stemmed from uncertainty in classifying valve problems. Even among cardiologists and cardiac surgeons this confusion can keep doctors from understanding each other and patients from knowing how to choose a qualified surgeon. Hilary’s specific difficulty would identify the type and complexity of lesions that her surgeon would likely encounter in the operating room and the level of surgical skill needed. And, critically, choice of surgeon would largely determine whether her valve was repaired or replaced. But so far, cardiologists and cardiac surgeons had focused solely on the state of her valve, not identifying choice of surgeon as a key issue in whether her valve would be repaired.
I also found expert opinions supporting mitral valve repair over mitral valve replacement. Dr. Bernadine Healy is a cardiologist and former head of the National Institutes of Health and the American Red Cross. She discussed severely leaking mitral valves like Hilary’s in US News and World Report, October 8, 2007. Paraphrasing, this article said that patients with repaired valves live longer, with better heart function and less risk of complications; that in the right hands, more than 90 percent of leaky valves can be repaired, though those in the U.S. actually getting repairs is lower, closer to 50 percent; and that most cardiac surgeons do only a few mitral operations each year, primarily replacements, mainly because replacements are what they know how to do well. Dr. Healy also said that repair surgeries require extraordinary knowledge and judgment; that tougher cases of mitral valve disease require the skill found in high-volume heart centers; and that if done properly, the fixed mitral valve functions almost as well as a normal one.
In 2006, the American College of Cardiology/American Heart Association (ACC/AHA) had published their Guidelines for Management of Patients with Valvular Heart Disease; they recommended MV repair over replacement for the majority of patients requiring surgery for severe, chronic valve leakage. The same year, surgeons in England drew the same conclusions (Ray et al, 2006).
With this encouraging information in hand, we focused on finding a surgeon who was skilled at repairing a severely deformed valve like Hilary’s and who could also advise us about timing her surgery. According to the British surgeons, to improve a person’s health, valve repair must eliminate valve leakage before onset of symptoms leading to heart failure. If a patient waits too long, even “normal” echocardiograms can mask significant heart muscle dysfunction and onset of symptoms may go unnoticed. Once a heart begins to fail, even if a successful repair follows, the patient’s life span is likely shortened. And when an operation occurs either too late in the course of the disease or as an emergency, repair is less an option and replacement more likely. Timing my daughter’s surgery required walking a very fine line.
Following our meeting with the cardiologists who told Hilary she needed surgery right away, HMO staff had stressed that the cardiovascular surgery department was “remarkably sophisticated.” But our choice of surgeons narrowed dramatically when we learned that only a few of them actually operated on heart valves. We selected the only plan surgeon who, by reputation, was skilled in mitral valve repair, with more experience at valve surgery than the others. His staff told us that patients came from all over the country for him to operate. With three long weeks until our appointment with this surgeon, and anxiety a permanent companion, I moved things forward from another direction.
I sent copies of two of my daughter’s most recent echocardiograms to a cardiac surgeon in New York City. Dr. David Adams is affiliated with a specialty, high-volume heart center such as Dr. Healy mentioned in her article, the Mitral Valve Repair Reference Center at The Mount Sinai Hospital. I chose Dr. Adams because I appreciated the quality of his writings on mitral valve repair. I asked if Hilary had Barlow’s disease, whether he thought she needed surgery, and if so, when? Most important, I asked if he considered her valve repairable. He responded quickly: Yes, it was a Barlow’s valve, she needed surgery, and, yes, in his opinion her valve could be repaired. He also said: “This is an operation for 2008, not 2009.”
I felt agitated that surgery seemed truly upon us, but calmed to know my daughter’s valve might be repaired. I admit to feeling a bit hesitant about his response, however, since Dr. Adams’ assessment countered numerous other physicians who had told us that her valve would likely have to be replaced, not repaired.
When we entered the most-experienced HMO cardiac surgeon’s office in January 2008, I looked forward to his estimate of best timing for surgery and fervently hoped to hear him say that she had a repairable valve. We had been told by experts that Hilary’s was not garden-variety mitral valve prolapse, but would this surgeon confirm Barlow’s disease? I assumed he would not only be familiar with Hilary’s records but also sensitive to a young woman facing open-heart surgery.
Wrong on all counts. He appeared not to have reviewed my daughter’s medical records. He fumbled through chart notes and could not make his computer work to study her echocardiograms. We sat expectantly. He gave her records a cursory look, then said she did not need surgery and should schedule another echocardiogram in six months. We stared at him. His statement contrasted sharply with other experts, many within his own organization who said she needed surgery now. He then said she had no symptoms and grimly added that surgery had many dangers and she “might have a stroke or die” during or as a result of surgery.
He reviewed a series of catastrophic possible outcomes in extensive, insensitive detail – failed surgery, death, loss of biologic function from stroke, heart or kidney failure, additional surgeries with unexpected outcomes, and on and on. We had lived with the fear of those possibilities for many years, but he spoke as if he was giving us new information. No one in her right mind would voluntarily undergo mitral valve surgery after his litany. Yet, in the face of these possibilities, and all too soon, Hilary would have to muster the emotional courage to tackle what only she could face: open-heart surgery.
Why did he focus on the risks of surgery, not the benefits? Delaying surgery, too, carried potentially grave hazards, but he said nothing about them. All the HMO cardiologists seemed concerned about my daughter waiting too long, but this surgeon did not. Did these people ever talk to each other? I felt stranded in the Land of Oz, baffled by the smoke and mirrors of the Wizard, invited to trust the man “behind the curtain” and give up what I knew to be true. I felt his opinion begin to erode my own judgment, based on knowledge from several sources, but forced myself to speak. I asked about “Barlow’s valve.” At first, he did not acknowledge the question, but a few minutes later, said off-handedly: “It might be a Barlow’s valve.”
Determined, I forged ahead with other questions prepared in advance – the what, when, why, and how. Surgery – when and why and how long does it take? Valve repair – what chance in Hilary’s case? Repair versus replacement – how many of each did he do in a year; what was his repair rate for Barlow’s valve? All important information to ask of any valve surgeon and essential to understanding what lay ahead. Certain responses would most likely lead to a timely and successful valve repair, others to delay and a replaced valve.
The surgeon’s answers all pointed toward delay. “If and when” Hilary needed surgery, he said, he was qualified to do it and valve replacement was a possibility – her valve defect was “complex and maybe too difficult to repair.” He spent time discussing the “several choices” we had for replacement valves. He then said she had only a 60% chance of successful repair, at best, and that he operated on two to three Barlow’s valves per year.
We knew that expert mitral valve repair surgeons at specialty centers repaired valves like Hilary’s two or three times a week, not two or three times a year. And their success rates were close to 100%, far above his predicted 60%. In addition, the surgeon’s focus on her lack of symptoms was a serious distortion, since lack of symptoms does not necessarily mean that a person’s heart is healthy. Even when a patient has no symptoms, the 2006 ACC/AHA Guidelines recommend mitral valve surgery in the following case: when her heart still functions well-enough, but she also has chronic, severe mitral valve leakage and elevated blood pressure in the arteries supplying her lungs. Since Hilary met all the requirements of these Guidelines, I had assumed that referral to a mitral valve repair center would be a mere formality, once the surgeon reviewed her records.
But as a result of his decision that she did not need surgery, the HMO would not approve referral. His short-sighted perspective checkmated our ability to seek outside surgical help and, perhaps, was not coincidental. We discovered later that he not only knew about mitral valve specialty centers, but had visited one recently. He chose not to tell us that much better options for Hilary’s treatment existed, forgetting or ignoring the part of his Hippocratic Oath that mattered most at the time: “I will not be ashamed to say ‘I know not,’ nor will I fail to call in my colleagues when the skills of another are needed for a patient’s recovery.”
Why did he give us misleading information? Was he careless in his assessment of her heart condition or simply out of touch with current medical thinking represented by the ACC/AHA Guidelines? Was he not clear about what he did not know? Alternatively, was he clear about what he did not know and, consequently, did not wish to operate on a 28-year-old woman with a severely-distorted valve he knew he could not fix? Was he motivated politically to use “lack of medical necessity” to deny referral and save his organization money? Ultimately, the reason did not matter. His lack of action protected his status and his organization, but put Hilary’s safety and well-being at risk. As a mother determined to protect her child’s health, I could not accept his judgment as final.
We now had two simultaneous challenges: first, to prove to our HMO that she needed surgery as soon as possible and, second, to search for a qualified mitral valve repair specialist who could mend a Barlow’s valve. All this while facing our own emotional reactions to her impending open-heart surgery.
I arranged for additional opinions from surgeons with four major mitral valve repair centers throughout the United States, each surgeon considered an expert at repairing Barlow’s valves. I asked them the same questions I had asked the HMO surgeon. Each confirmed that surgery should happen soon and that repair was likely. Hilary chose the hands she wished to fix her ailing valve.
We requested an out-of-network referral from the HMO’s Medical Center Review Committee. Our request cited supporting medical and surgical opinions, both inside and outside our HMO. It accompanied a labeled, cross-indexed binder, containing our previous correspondence with the HMO, letters from the consultants that clarified Hilary’s deteriorating condition, and copies of literature documenting the need for surgery with a qualified surgical team. The Review Committee, a group of administrative personnel and physicians who are not cardiac surgeons, would decide if open-heart surgery was “medically necessary” and whether to grant referral to an out-of-network facility. The reviewers consulted the cardiovascular surgery department at the HMO, but did not consider the opinions of the HMO cardiologists – the ones who said Hilary needed immediate surgery.
Within days the HMO Review Committee officially and firmly denied our request for out-of-network referral. They said there was “lack of medical necessity” and that their organization had “appropriately privileged and credentialed physicians available to provide this service,” if and when necessary.
The Committee referred us to another surgeon inside the HMO’s cardiovascular surgery department for a second opinion. No surprise that the “second opinion” was in concert with the first. Surgery wasn’t needed, he said, adding that he, too, was qualified to perform valve repair, if required. When I asked specifically about his statistics for Barlow’s valve repair, he said irritably, “My statistics are great.” I persisted, and eventually he said he did not know for sure what his statistics were, because “if the surgery didn’t go well, I wouldn’t know because the patient wouldn’t return to me, would he?” Presumably the patient died. If this comment was meant to be funny, it failed – we knew that this cardiovascular surgeon had even less experience with mitral valve repair surgery than the first one.
The Chief of Cardiovascular Surgery gave a third opinion. He never met with Hilary, and he agreed with his colleagues.
After three denials that spanned seven months, I felt stumped and again doubted my own hard-won understanding. Had they seen something in the data that I had missed – something that proved Hilary’s situation was not so bad and that she should wait? For my own sanity, I put together a simple chart of her heart measurements, from age seven to the present. The changes were unmistakable, even to a non-M.D. like me.
I contacted San Francisco attorney Arnold Levinson, who had guided our communications with our HMO and, in his unlimited graciousness, not charged one penny for his help. I told him we’d had our final rejection from the HMO, that my newly-created chart of numbers showed we were right about the changes in Hilary’s heart, and I guessed it was time to contact the State Board of Managed Health Care for an Independent Medical Review. “It’s premature,” he said. “Why are you letting the word ‘final’ get to you? If you have new information, your HMO is legally required to consider it.” He then asked about my chart of numbers and whether I could think of one more person in the HMO to meet with – one person to show my numbers, who might be willing to help.
The chart by now had become a folder; here are a few of the relevant numbers.
- Echocardiogram 12/27/07: LVID, d 6.5 cm
- Echocardiogram 01/08/08: LVID, d 6.2 cm
- Echocardiogram 02/25/08: LVID, d 5.80 cm
- Echocardiogram 05/21/08: LVEF: .55 or 55% – moderately severe mitral regurgitation
“LVID, d” = Left Ventricular Internal Dimension. When the heart is working too hard the muscle grows thicker, and the internal dimension shrinks. This reduces the ventricle’s capacity, which is not good.
“LVEF” = Left Ventricular Ejection Fraction, a measure of how well the heart is pumping out the blood.
I mentioned a retired surgeon. “Go see him,” said Arnie.
We told the surgeon that we had gotten such a range of opinions we didn’t know what to think. Initially, he stonewalled. But as he saw Hilary’s clear distress and, finally, looked at my chart of numbers, he paused.
I said, “We need to know whether this is the time for surgery.” He nodded. “It’s time?” I asked. “Yes, you are in the window when it needs to happen.” Hilary and I both dissolved in tears. After a moment to gather myself, I then asked the second big question: “Should her surgery be done by the HMO?” “No,” he said, “we cannot do that surgery.” He said referring Hilary to a specialty center focusing on Barlow’s valves would be comparable to referring heart transplant patients to an outside center specializing in transplants.
Within hours of submitting the new information, my chart summarizing years of data and the retired surgeon’s opinion, the HMO rejected it, saying, in essence, “What part of ‘final’ don’t you understand?”
This event triggered our last appeal, to the State Board of Managed Health Care. The board referred it immediately to the Center for Health Dispute Resolution (CHDR). Within ten days of receiving my request for an Independent Medical Review, the CHDR overruled our HMO’s denials. They cited the extensive case file, including all the letters, expert opinions, and research materials that no one in the HMO seemed to have read. The CHDR then said that due to severe Barlow’s disease, Hilary needed a complex repair, that only a specialist was qualified to perform it, and that the surgery was medically necessary.
Against all odds, we had succeeded, through stubborn perseverance, self-education, and self-advocacy.
Within days, the HMO contacted Hilary about travel arrangements and lodging while recovering from surgery. Less than a month later, Drs. David Adams and Ani Anyanwu, at the Mount Sinai Medical Center in New York City, successfully repaired Hilary’s mitral valve. Her heart valve function is now essentially normal. It no longer leaks, and she has her life back. You might say Hilary found her pair of ruby slippers, in spite of the Wizards’ misguided attempts to keep them from her.
Dr. Adams has referred to the increasing opportunity for mitral valve repair as a “revolution.” The late mythologist Joseph Campbell said, “Revolution doesn’t have to do with smashing something; it has to do with bringing something forth.” If mitral valve repair ‘brings forth’ the patient’s ability to live a healthy life, with her own repaired valve, then they are both correct.






Congratualtions! What can one say but determination goes a long way!
Thanks, Alexandra. It was quite an odyssey. I appreciate your comment!
Warm Regards,
Diane
I forgot to say, Diane is VERY committed to helping others in a similar situation; she asks that people contact her at diane at dianeengelman dot com.
Wow. What a story…incredible persistence AND intellect in caring for your loved one.
BUT, I’m left asking myself “How many people would have both the level of persistence and intellect as mama lion…how many aren’t getting optimal care?”
Thanks for your comment, Vince. I worry too about people not getting the care they need. And, I know from the experiences of myself and others, persistence is the most critical. Coupled with with a healthy sense of entitlement and willingness to seek support from others, perseverance is what brought me through.
Warm Regards,
Diane
Diane, What a blessing for Hilary that you are intelligent, persevering and not intimidated by the strong and sometimes paternalistic world of medicine. I shutter to think of what other families might fall victim to, lacking a similar “voice” and confidence to stand up and speak your truth.
Thank you for sharing your story so many of us can feel empowered!
Hi, Anna –
Thanks for your comment. Finding and keeping my “voice” was a bit of a moving target. I fell apart regularly, but, with my daughter’s health weighing in the balance, it was amazing how quickly I would re-find my “voice.” I survived the ups and downs of this odyssey with the help of loving relatives and friends.
Warmly,
Diane
Having known Diane for a long time (probably longer than she will care to admitt) her persistance in advocating for her daughter does not surprise me one bit. Having been forced to experience two different, but similar situations, I can honestly say that both patients and family must not stand by and take what Dr.’s, hospitals, or insurance companies try to mandate if you feel that there is a better way to follow. Congratulations Diane. I’m proud of you and happy for Hilary that you’re her mom.
We go back a long time, Marshall, and I appreciae your continuing support.
Diane and JB,
Thank you for sharing this wonderful account with the rest of us. I had seen an earlier draft but just read this version and found it terrifically inspiring. I see this as a tale that goes beyond medical advocacy–it’s about the power of love and about the need for each of us to listen to our inner voice and not just accept “what is”. I am going to try to practice this in my own way.
Thank you for sharing your thoughts, Steve. You always bring heart to a discussion. Therapeutic Assessment is your version of unique “patient” empowerment. I have learned much from you.
Without people like you, people who don’t understand the meaning of “final,” we would all be in trouble!
This story holds so many important messages. The one that strikes me most: doing independent research is essential. Even the best and most well-intentioned doctors may not be up on all of the latest information. By being a determined, diligent patient, you help subsequent patients as well as yourself.
Thanks, Barbara. You were more help than you know while I was writing this article.
I am a pathologist, far from this area of expertise, but did extensive research on this subject for a friend in a similar situation. I think this HMO’s behavior borders on malpractice and should be reported to whatever governing board is available. Mitral valve repair is NOT a new type of surgery and is currently the standard of care unless there are contraindications – which are rare and do not seem to be fulfilled in this case.
In my friend’s case, his own cardiologist, despite practicing in a hospital with a cardiac surgery program, recommended he go to the Cleveland Clinic. 3 years later, he is healthy. I am glad your daughter had a similar result, but I would not let this go for other patients’ sake.
Dear bev M.D. –
Thank you for your thoughtful response. I am carefully thinking about your post.
I sat outside the National Institutes of Health this morning, reading this post on my Blackberry while waiting for my meeting with the directors of communications to begin. The line that resonated with me: “I chose Dr. Adams because I appreciated the quality of his writings on mitral valve repair.”
Thank you for the inspiration to talk with renewed clarity about the power of opening up science, opening up communication, opening up journals.
My message today was: “Information is currency and the NIH is a bank. Open up.” A fantastic discussion ensued – I’ll write more about it later. For now: Thanks.
Susannah – I am touched that you were inspired by Hilary and my experience and our ability to communicate it. Please stay in touch.
I have known Diane for years now – and even though I have heard her story before – I’ve never understood it like this. What am amazing mama lion you are Diane – Hilary is so very lucky. If I can half as strong as you if that time ever comes…
Angela, thank you for your comment. I’m especially happy to hear “I’ve never understood it like this.” On this blog we try hard to make understanding accessible to people – can you say anything about how / why this story worked for you?
I appreciate you, Angela .. you have helped me understand the power of social media and web site communications. I look forward to on-going work with you.
like the aformentioned mr. johnson i have also had the distinct pleasure of knowing diane for many years. and i am not surprised by her determination, strength, courage, and tenacity in the advocacy for her child’s health and well being! after all, isn’t that part of the definiton of motherhood? but her success in the face of such resistance is to be commended, and her reward comes from the love and admiration of a healthy child….and many, many friends!
Hey, John –
Thank you for your lovely comments. And, thank you for making me laugh at every possible opportunity.
Diane — just off the redeye from Oakland to JFK. Checked my email and found this link from you… rereading your story (with so many more details) reminds me of two things: 1. that there are truly hero loved ones – like you! – who advocate for the people they love, joining the ranks of e-patients in the process and 2. that we still have so very far to go. Why is it that America has the best medical care available in the world – but we have to fight so d*mned hard to get it?
Lest this evolve to a rant, when I’ve had no sleep and too little coffee… please give Hillary a hug, and ask her to click the heels of those ruby slippers. And thank YOU for sharing your story.
Trisha Torrey
Trisha,
In my haste to post this I failed to note that Diane already was quite familiar with your site and your excellent (and very appropriate) book You Bet Your Life: The 10 Mistakes Every Patient Makes. Rant or no rant, you are a pioneer of patient empowerment and deserve wide recognition.
It’s hard to believe I met you only 13 months ago at “Health 2.0 Meets Ix.” Feels like I’ve been cousins with you forever.
Trisha, Your book, You Bet Your Life The 10 Mistakes Every Patient Makes is fabulous. As each one of us, as consumers of medical care, becomes more savvy about health care delivery in this country, we will make fewer mistakes, achieve better services, and change a very broken system. Thank you again!
Diane–Great story. But you’re not doing anyone any favors but not naming names. Who were the doctors? Which “HMO” was it? Where? Which department? Which state.
I assure you that you’ll have much more impact if you make this all public. And if it’s who I think it is, there are people in that organization who will be on your side.
Thanks, Matthew. I appreciate your thoughts and am carefully thinking about your words.
Sorry minor typo in my comment, I meant
“But you’re not doing anyone any favors BY not naming names.”
Please consider. It’s not just naming and shaming–it’s a chance for a real debate.
Hi, Matthew –
Tell me what a real debate would look like.
D
Diane–If you named names, then both the doctors and the organization would have to engage, tell their side of the story, and defend their actions. They may actually have something worthwhile to say.
For example, the larger organization may be unaware of this department’s practice. There may be factions inside the organization that need a case to advance a better way. If not, pressure can be applied if appropriate. Or maybe your side of the story is wrong.
You know who they are–they know who they are. The only reason to not tell the rest of us would be that you have a financial settlement contingent on not talking. And if that’s the case you should reveal it.
If you don’t rewrite this with real names, this is a great story about how you were a fierce advocate for your daughter. But you haven’t changed the wider process, and what happens to the next daughter whose mother isn’t as tough or smart as you?
Matthew
Hi Diane:
As I always tell you…..you never cease to amaze me.
So happy you finally achieved getting ‘this article’
published. I certainly know the time and effort that went into writing it. Last, the ‘MAMA LION’ title is very fitting!!!!!
Congratulations, Bill
Thanks, Bill. Thank you for your part in keeping my garden happy while we lived through Hilary’s medical saga. You are a true friend.
If this doesn’t define perseverance, I don’t know what does! While I know the strength of both of these women, I am even more amazed and impressed by the “sticktoitiveness” that you demonstrated AND trusting your gut that what you heard wasn’t the whole story. Fantastic job of wading through the myriad of information available on the internet and using your instincts and saavy to zero in on the right source for help. I’m so glad the right angels were sent your way and your heart(s) remained open to hearing them and keeping you true to your course. We are all blessed that both you and Hilary are here with us to share this journey.
Thanks so much, Annie. I’ve missed seeing you two.
Diane:
Having known you for as long as I have, your intelligence and tenacity does not come as a great surprise. What an inspiring story! Even better, what an inspiring, happy ending to a grueling saga. As you know, I have handled numerous medical malpractice cases over the years and it is tragic when lives are lost or medical conditions made substantially worse because of what I perceive to be either indifference or a frequent preoccupation for economic over therapeutic interests by those individuals and entities charged with a person’s most precious possession, . . . their health and well-being. Hilary is fortunate to have a mother with the willingness not to take “no” for an answer, and the intelligence to be able to thoroughly substantiate her position when challenged. Congratulations on a well-earned victory and my best wishes for continued health and happiness to you and Hilary, Dave
Thanks,Dave. So great to hear from you!
Diane-
I so appreciated being able to read the entire journey–written with so much head and heart and persistence. You are at the top of my list of lion mothers—and gentle people. Thank you.
Deborah
Deborah, thanks so much for pointing out that persistence and insistence can absolutely come from a gentle person. This is in no way about being a jerk – it’s about standing for what’s right, which can come entirely out of love.
I’ll go a step further.
Most of my speeches start with a slide on “Foundation Principles,” including:
– the right of a desperate person to save themselves
– the right to know what your options are
– the right to take your data pursue an option elsewhere.
How dare anyone say it’s wrong or rude to insist on good care? How dare anyone block information about the best available treatments, and block access to them? Social norms like that are harmful, and must be torn down.
Hey, Deborah –
From one Mama Lion to another … I say thank you for your comments and for reading this long journal account of our odyssey. While gentleness is at times a virtue, it also is a liability. Finding a balance in this particular experience was a challenge for me. I found my way by orienting and re-orienting myself along the path so Hilary was assured of getting necessary and appropriate surgical care.
What a inspiring story. You are a great mother Diane. I am so happy you perserved. Your story shows how difficult it can be to advocate for ourself. You are truly a Lion mother!
Congratulations on Hilarys surgery!!! You must feel fabulous to have won the battle.
Thank you Karen for your post. Advocating for Hilary was certainly a process not an event. I was able to succeed with the support, love, and guidance of many family members and friends.
Hi Diane:
The most important message in your terrific article is the importance of keeping your eye on what really matters — Hillary’s chance to live a normal, healthy life in the face of a debilitating condition. It is impossible to know what was going on in the minds of the HMO cardiologists who evaluated Hillary and it is to your credit that you didn’t get hung up on their personalities and motives but rather sought to always move forward and advocate for Hillary. It is sad when medical ethics and business ethics clash as they did in Hillary’s case. At the same time it is hearening to see that there was an option available to force the HMO to do the right thing for the right reason. Your story is an important one to tell not only for you, Hillary and your family, but for all patients and families who find themselves in the same situation you did in 2003. Thank you for sharing it in such a deeply personal, yet comprehensive way.
Hi Rick –
Thank you for your thoughtful message. Medical ethics and business ethics do clash. It’s amazing to me just how far away from simple human caring we’ve come in our culture. It’s particularly poignant and unsettling in the medical arena.
In the article JB Allyn and I wrote, the following quote sums this medical lack of caring up: “He chose not to tell us that much better options for Hilary’s treatment existed, forgetting or ignoring the part of his Hippocratic Oath that mattered most at the time: ‘I will not be ashamed to say ‘I know not,’ nor will I fail to call in my colleagues when the skills of another are needed for a patient’s recovery.’”
I believe better times are coming. It will take many voices, much dialogue, deep soul-searching by all of us, and a solution-oriented focus.
Hey Diane,
What a journey! Hilary will have a great story to tell your grandchildren thanks to you.
Who knew there was a real Dr. House, and you found him.
It doesn’t matter which HMO you went to, they’re all the same. Your story is a great example of our broken health care system. I hope it woke some poeple up.
HKBR
Heidi, nice to meet you.
I just want to add that it’s a bit of an overgeneralization to say “they’re all the same.” When I was in the pits with my cancer (very bad odds and expensive to treat), my insurance company (Harvard Pilgrim at the time) was excellent.
Now that I think of it, the 5th blog post I ever wrote (December 9, 2007) was titled Thank You, Harvard Pilgrim.
It’s great to hear such a positive story about health insurance, Dave. Thanks.
Hi, Dave –
Tell us more about your insurance carrier Harvard Pilgrim.
Heidi –
Thanks for taking the time to read the article and comment. I wish I knew more about the good health insurance stories e-patient Dave mentioned.
I thought I knew your story Diane, but obviously not well enough. This will inspire many of us to start thinking more ceatively about our medical care. The tenacity it takes to do this in the context of everyday committments is extraordinary. Hilary has an amazing mom, and has clearly benefited from your perseverence. Thank you for leading the way.
Hi, Disty –
And you were an important member of the support team! Thanks!
My friend, Joyce Anis, sent this to me and I plan to forward it to the Utah Health Policy Project. They are always looking for stories like this.
This is why we need Health Care Insurance Reform. The current law is only a baby step in the right direction. Unfortunately, as long as the USA is wedded to the market as the provider of health care insurance these type of problems will continue to happen. When business profits come up against the best health care option for the patient all too often business profits trump health care. This is more true for the for-profit health insurance companies that for the non-profit health insurance companies. Back in the 70’s I had hope for HMOs as a solution to this problem, but the bean counters took over the HMOs and perverted the idea that the medical professionals would direct patient care. I guess I will just have to keep praying for a “single payer health insurance” that contracts with any qualified health care professional and allows the patient to choose the one that meets their needs.
Dear Kathleen –
I’m glad you are sending the article on to Utah Health Policy Project. Thanks. In this case, business profits did not triumph over health care. It took too much effort to make that happen… but I am grateful it did. The State Board of Managed Health Care saved the day.
Bravo Diane!
I have always admired your smarts, your tenacity, your compassion and your commitment to mothering. These qualities and much more is what it took for you to negotiate your way through the maze of medical Alice in Wonderland and emerge with a reality that worked for Hilary in the best way imaginable. Your story truly inspires others to keep fighting for what they need for themselves and their loved ones.
Your friend,
Michele
Kathleen, are you mad? Health Care reform will institutionalize the Engelman’s experience for all, mama lion or no mama lion. We’ll all be in one big HMO, only stupider and more arrogant, and with no appeal possible – as are NHS patients in the UK.
Only the existence of a market, however impaired, makes centers like Mt. Sinai’s possible for those who can afford it, or who have the intrepidty of the Englemans. Such centers of excellence don’t exist in the UK or Canada – we should cherish them while we can, support them with our dollars and our votes and our business, and most of all, use our heads. We must understand that we must break down the walls that insulate incompetence and mediocrity like that which the Englemans’ HMO embodies, rather than layer them in layers of bureaucracy that are impervious to human feeling.
Thanks – I printed out a copy to read later!
Just read your story. my daughter will have to have this done soon. When is the question? We see the doctor tomorrow for an exam. It will be good to know all of what you have been through. I now know that a valve can be FIXED, not replaced. Thanks
Hi, Dave –
Thank you for helping me to post Hilary’s story. We want others to know that they too can successfully advocate in the medical arena to find the care they need and deserve.
Warmly,
Diane
Yeah!!!!!!!!!!!!!!!!!!!