Prepared for Mayo Transform 2010: Thinking Differently About Health Care (video now available).
Ten years ago, I wrote the Pew Internet Project’s first report on the impact of the internet on health care, calling it “The Online Health Care Revolution.”
Back then, the idea that people were searching online for health information was revolutionary. All of a sudden, regular people had access to medical information that had always been locked up and out of reach.
Ten years later, I am ready to declare the access revolution over, at least in the United States. It’s time to change our frame of reference. Instead of talking about a revolution, our data shows that it is time to start building a new civilization. The Mayo Clinic was a leader during the revolution, opening up your expertise to the world. You can continue to be a leader if you take advantage of the trends I’m about to share.
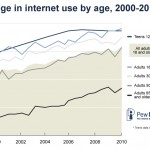
In 1995 only about 1 in 10 American adults had access to the internet. This was not that long ago. In 2000, it was up to nearly half of adults. Now, about 75% of adults and 95% teenagers in the U.S. have internet access.
Notice that lower line: the 65+ age group. There is a steady climb of internet users, from teenagers up to baby boomers, and then a cliff at about age 70-75.
There are still pockets of people who remain offline, the most significant group being our elders, but many of them have what we call second-degree internet access. Their loved ones are online.
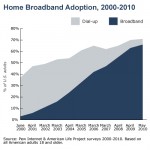 In the year 2000 only 5% of households had broadband access. Now, two-thirds of Americans have broadband at home. Another revolutionary hurdle passed. One Pew Internet study found that dial-up users take part in an average of 3 activities per day. Broadband users take part in 7.
In the year 2000 only 5% of households had broadband access. Now, two-thirds of Americans have broadband at home. Another revolutionary hurdle passed. One Pew Internet study found that dial-up users take part in an average of 3 activities per day. Broadband users take part in 7.
82% of American adults have a cell phone. Six in 10 American adults go online wirelessly with a laptop or mobile device.
Mobile was the final front in the access revolution. It has erased the digital divide. A mobile device is the internet for many people. Access isn’t the point anymore. It’s what people are doing with the access that matters.
Pew Internet research shows that mobile + broadband adds up to much more than 1+1. Each one has a multiplying effect on people’s behavior.
Let me give you some more context: How many of you remember your favorite class from your first year in college? Mine was Geology 101.
Our professor knew that very few of us were going to study rocks or soil samples, so he made it his mission to make us see the landscape in new ways.
His advice makes sense, and not just as a geologist: Know the history of the land you live on. Know that you can’t escape the reality of the landscape, but you can adapt to it.
Geologists are trained to take the long view, to notice patterns and to apply those observations in immediate, practical ways. That is essentially what I do today: I’m an internet geologist.
So where’s the action? What is causing the most radical landscape shift online? Wireless access.
Mobile devices are changing us, once again, as internet users, making us more likely to share, more likely to access information on the go, and, as I mentioned, erasing the digital divide. Once information is untethered, the oceans part and the landscape changes. We are now on the other side of a massive shift in communications.
In 10 years we have seen the internet go from a slow, stationary, information vending machine to a fast, mobile, communications appliance that fits in your pocket. Information has become portable, personalized, and participatory.
In fact, as we have watched the rise of wireless access, we’ve identified an effect that we’re calling “the mobile difference.”
Once someone has a wireless device, they are more likely to use the internet to gather information, share what they find, and create new content.
If your organization’s information is not available on a small screen, it’s not available at all to people who rely on their mobile phones for access. That’s likely to be young people, people with lower household incomes, and recent immigrants – arguably important target audiences for public health messages.
Mobile makes things personal. Mobile makes things immediate.
Just how immediate? One study in the Netherlands found that the average response time to a text is under 3 minutes. That’s an incredible opportunity. Let’s call it the FedEx principle. A FedEx arrives, you open it right away. A text message arrives, you open it. Text messages are personal, immediate, and tailor-made for calls to action.
For teenagers, you can multiply the FedEx principle by a factor of 10. Here is how this can be harnessed:
A team of Stanford researchers, working with Project HealthDesign, wanted to help chronically ill teenagers take more responsibility for their health.
In talking with teens, the researchers found that technology is a comfort, especially if it is portable, like an ipod or cell phone. They also found that teens are less likely to take their meds if they are feeling sad. So the researchers came up with a tool that tracks the teens’ moods, monitoring the songs they listen to and the words they use in text messages to friends and family.
And the teenagers agreed to surveillance? Yes. For two important reasons: #1, the researchers were a trusted entity. #2, it was a trade-off they were willing to make for better health and more independence from their parents.
The teens wanted to break the cycle of being in a bad mood, forgetting their meds, and catching hell. With the new tool, listening to sad songs or texting negative language triggers a medication reminder. The messages were seamlessly integrated into the teens’ lives, increasing their treatment adherence. And mom had nothing to do with it.
Treatment adherence is a huge challenge for health care today. Think about how the Mayo Clinic, another trusted entity, could harness a tool like this one. Look past the old conversations about privacy when you’re building on this new frontier. You may find creative solutions that get results.
On the other side of the age spectrum, the Pew Internet Project just released a report showing that older adults are flocking to social network sites, which is kind of a man bites dog story and made a lot of headlines.
But look at the uptake of these sites among young adults: 86% of internet users in their 20s use Facebook, MySpace, or LinkedIn.
Some of this data won’t be surprising to you, but we think it’s important to have the numbers, so we can look for new patterns.
For example, Pew Internet surveys show that social sites are becoming important hubs for health advice. People want to learn from each other, not just from institutions.
You might worry about people are giving each other medical advice. That’s got to be dangerous, right? So far, no. We’ve asked people in our surveys: Have you or someone you know been helped by health information found online? 60% of internet users who go online for health say yes, which is up from 31% in 2006. We’ve also asked: Have you or someone you know been harmed? That’s a flat-liner at 3%.
Here’s your opportunity: people are still often looking for, and linking to, authoritative source material. Make it easy and attractive for people to link to you. Seed the online conversation with data, with science, with evidence. You can’t control the conversation, but you can be part of it.
In addition to the “mobile difference,” by the way, we have also identified a “diagnosis difference.” Our research has found that internet users living with chronic disease are likely to be older and living in lower-income households – people who generally stay in the shallow end of the online activities pool. Email, search.
However if we control for all those other variables, living with chronic disease increases the likelihood that an internet user will say they work on a blog or contribute to an online discussion about health. They are learning from each other.
The rise of social networking shouldn’t surprise us. It is part of the history of our landscape. It is an ancient, communal ritual to talk with each other. The bottom line is that the internet widens your neighborhood, expands your networks, and speeds up the pace of conversation. And people say they feel better because of it.
In an online survey we conducted last year, one person shared: “I was having problems sleeping [because of] hip pain. Through this [online health community] I received information about proper ways to set up my bed and since then have been sleeping so much better.” A simple change, suggested by a peer, and it happened online.
Another respondent wrote, “I read the Gluten Free Forum daily for about a year before I really got my celiac disease under control and felt fully informed. You can’t call your gastroenterologist every time you buy a new product.” That’s where health care happens – in the grocery store aisle, making a decision, wondering what to eat for dinner tonight, looking up choices on a smartphone.
Think about what would happen if we could harness the instinct to share with the tools to make it easy.
About 20% of the online health population has posted comments or content related to health care. That’s the classic Pareto principle or 80-20 rule – 80% is listening, 20% is talking. But here’s where it gets interesting: hand someone a smartphone and they are more likely to become a contributor, a commenter, a creator. Mobile access bumps up participation.
What will happen when the untapped knowledge of every patient, of every caregiver, of everyone who has something of value to share actually has the opportunity to share it?
That’s the next frontier. It is no longer about access. It’s about uploads. It’s about inputs. It’s about learning from each other.
Patients are not the only ones who can benefit from this new model of participatory medicine. Institutions can too.
E-patient Dave deBronkart is a tech geek who also happens to be a cancer survivor. He used CaringBridge during his illness to stay in touch with his friends and family. He used ACOR to gather expert peer advice about kidney cancer. He used Beth Israel’s PatientSite to keep up to date on his treatments and communicate with his doctors.
So when Beth Israel announced a partnership with Google Health, Dave was among the first to press the button and allow his medical record to get sucked into Google Health’s online system.
Unfortunately, the system transmitted everything Dave had ever had – and a few things he’d never had. With almost no dates attached. It also sent through every medication Dave had ever been on, triggering a scary medication warning that was absolutely irrelevant and wrong since he hadn’t taken that drug for two years. Turns out that the system transmitted billing codes, not doctors’ diagnoses, and nobody had ever really looked at the results.
Well, until Dave blogged about it and his story was picked up by the Boston Globe.
As an internet geologist I’d have to say that Dave was a one-man earthquake, taking Google and Beth Israel by surprise.
The good news is that both Google Health and Beth Israel welcomed Dave’s critique and have made changes to their systems. But I bet they wished they’d done a test run with a group of patients before Dave published his post. Now Dave lectures around the world about how patients want to help and how patients want to be part of the new model: participatory medicine.
Let me wrap up with a couple of thoughts, going back to looking at the landscape and what it tells us.
The access revolution is over. Mobile is changing us, changing our frame of reference so that we see information as portable, personalized, and participatory.
Health care has a marvelous opportunity tap in to our ancient instincts to share and our modern ability to do so at internet speed.
Build on the new frontier. Build on the power of mobile.






How can there be no comments on this post??
I know: it’s because this is such a blindingly bright revelation, there’s nothing left for us to say. (I’m not kidding – I was stunned long before the end.)
I have a huge concern though: “laptop or mobile” seems equivalent to “car or lawn mower.” A year or two back, my wife and I had phones with simple SMS and a simple camera. Then we got Blackberries, for separate reasons, and started carrying email in our pockets, along with a pretty feeble browser. Now she’s got a DroidX, which dwarfs a Blackberry in its power as an information appliance in her pocket.
Where does Pew draw the line? What’s “internet access” and what’s not? You say to format for a small screen; how small?
Because if we’re talking about erasing the digital divide, what she now carries sure won’t reach down into the lower economic tiers – not this year, anyway.
Do you cross-tabulate with data from the cell phone industry about device adoption, especially by demographics? What can you project about iPhone/Droid-style screens, 1-3-5 years from now?
Colossal post.
p.s. I love “revolution’s over, start building the new civilization.”
Dave et al,
You are asking a very good question that’s going to take me a day or two to research and answer… but I will.
Oh, and if anyone is impatient, please know you can dig in to Pew Internet data for yourself. We upload all of our reports AND our data sets for free on our site.
Here is the latest survey, from May 2010:
http://pewinternet.org/Shared-Content/Data-Sets/2010/May-2010–Cell-Phones.aspx
You only need Word to look at the questions & the crosstabs. We upload the SPSS file for the serious geeks.
Mobile health and mobile learning are two disciplines that are rapidly developing and those in both fields need to recognize how to develop synergies to create the most effective apps. (Just a reminder that those dipping into #mhealth on Twitter should also be checking out #mlearning and visa versa). Not every health app is a learning app but many patient-centered ones are.
It would be interesting to see data on how many actually have smart phones (vs mobiles with internet access). But even with just internet access and texting, a lot of creative things can be done.
A lot of people have been pushing, coaxing, encouraging and screaming about the explosion of mobile for past couple of years, particularly when it comes to those underserved demos in healthcare you mention…and so much more.
Thanks for putting it out there so eloquently and persuasively.
Love your advice: “Know the history of the land you live on. Know that you can’t escape the reality of the landscape, but you can adapt to it.”
Daphne
Thanks so much, Daphne! I could talk for days about my geology professor – he had a wonderful Scottish brogue and was clearly a philosopher who happened to study rocks. It’s only [lots of] years later that I’m really coming to grips with all that he taught me.
Dave is right,
for some time a barrier-to-care will exist in regards to accessing information and participating. Smartphones come with hefty contract prices and while their proliferation continues to spread rampantly, it will be years before those that might benefit the most- the elderly and the impoverished- have access to or seek out these devices.
I would also be interested to hear if anyone has suggestions on methods one might use to direct friends and loved ones to information sources which could help them make changes in their life (i.e. better managing celiac disease). While their life is not ours to live, I think we all know someone that could benefit from learning more about making healthy choices or better managing their condition.
Chris
Thank you for this post. I must have read the part about small screen information availability three times. Then, after reading: “…young people, people with lower household incomes, and recent immigrants – arguably important target audiences for public health messages.” I agreed with e-patient Dave’s comment on device adoption demographics. What are the stats on the correlation between household income and smart phone ownership?
Thank you again for this post Ms. Fox.
What a great post! I can see possibilities for targeting underserved populations via social media. Already, Merck has launched a diabetes iPhone app that uploads basic vitals and provides mentoring on disease maintenance while also allowing for direct doctor-to-patient contact. What is missing is a gaming component to bring in younger teens to make adherence fun. We are at the begininning of real participatory medicine and it is quite exciting.
Thank you for the comments so far! I am thrilled by the questions I received at the Mayo Transform event and here. I am traveling back to DC at the moment and will jump in to the discussion tomorrow. Again, thanks – this analysis was a long time cooking, with much help from my Pew Internet colleagues.
Great article, Susannah and points absolutely well taken. In this regard I completely agree with Dave.
With regard to the adoption rates of mobile smart phones by those in a lower socio-economic category (as alluded to by Sarah, Dave and Chris) I have a slightly different take.
Cell phones are currently ubiquitous across all socioeconomic classes. Indeed, for many, it is economically preferable to have a mobile number and to avoid a land line entirely. Broadband access to mobile devices is (and will continue to) have a decreasing price point.
Rather than seeing the the future of smart phone adoption going along the path of expensive options like an iPhone (via AT&T) or the Droid X (Via Verizon) I would like to think (and hope) that young entrepreneurs will take advantage of existing technologies and leverage open source software to make robust smart phone software available to anyone who can afford even a pay as you go cell phone. We are not there yet. Android phones (like the Droid X) feature an open source operating system and an open market but the up front costs and commitments remain out of range for many.
But I’m actually encouraged by the sophistication I’ve seen in cell phones carried by individuals in the developing countries I’ve visited (Nigeria, Ghana and India).
Hopefully, there are innovators who will take the opportunity to provide smart phone technology which will affordably bridge the digital divide.
I just heard Susannah present this material at the Mayo Transform event – it was a very good 15 minutes (the talks were all short). I am a biotech-academic scientist, and after her talk I asked Susannah two questions, sort of: first, I wanted to know her thoughts (and still do) regarding the difficulties people have making choices when the language of medicine is so difficult (or is made difficult to make decisions more difficult – I am sure that is part of it), and then I also wanted to know what thoughts she had about the evidence-based paradigm we all like for modern medicine, even though we seem quite unable to define what evidence we might like to use in decision-making. Both questions are large, in my mind.
One task (the easier one) that all medical scientists share is to make language as clear as possible so that untrained but logical and thoughtful people can make informed choices. The more difficult (and more scientific) question is what evidence ought to be used by those same people to make choices, and this one is tough because even the “professionals” have not yet had that discussion deeply.
Modern medical science is getting closer to “knowing” about what evidence matters for which medical conditions, but the ability to communicate with people is available right now, before even the experts are sure what evidence to throw into the discussion. This was inevitable – electronic stuff is kind of easy, and biology is very difficult and strange. The gap between communication and medical data had to exist, and does.
Glad to have joined this discussion – it is my first time ever to add comments to such a forum. Very odd indeed.
I’m so happy to see comments from new names here! Love it when the community grows, especially when people move from passive consumer/reader to active speaker-upper. (Those aren’t technical sociologist terms.)
Larry, I have a strong sense that a driving factor in simpler vocabulary will be market mobility: when it’s easy to take your business to a provider who speaks your language, more providers will start doing that. We’re mostly impeded today from doing that.
Here’s a wacky thought: what if we-all, the public, created an open, open-source PHR, to compete against the big-iron vendors? What if Mozilla (open-source makers of Firefox etc) created Welby, a personal health record named after the old TV show Marcus Welby MD? Its feature set would be determined by what users want, and special-interest groups could create plug-ins and modules for specific needs. And it would be all full of APIs, to send and receive data.
For sure its data model would be completely distinct from presentation (browser etc), i.e. it would be designed from the ground up to do well on smartphones. And I bet it would make use of thin, useful methods well suited to plain cell phones, like the one Alan Viars discussed last winter.
What do y’all think?
Larry, thank you so much for jumping in to this new space and posting a comment!
I was at first taken aback by your question at the event and then intrigued. I want to think about it for a bit before I try to answer — yours was definitely an “after-speech” question that deserves everyone’s attention, not just mine.
Let me say it here–mobile is dead. For that matter the web is dead, as Chris Anderson just said. Of course people will use all manner of devices, but there isn’t one strategy for getting to any one person. Not even the mythical text-only Dutch teenager. They’re also on Facebook, iPhone & Android apps, in walled gardens, using open source tools, etc, etc–not to mention still paying attention to email-based listservs, oh and seeing flashing pill boxes, and receiving automated phone calls that they prefer to human ones.
Health care people who want to get to health care consumers need to be everywhere and LINKING the data created and received to each other–over any unplatform.
Susannah’s geology lesson is fantastic. But it’s a geology lesson. It’s not a blueprint for the future.
Sir Matthew of Holt,
I find it hard to imagine that the omni-everywhere behavior you cite is prevalent in the socioeconomic groups where disparities are common, and people like Aligning Forces for Quality are working to eradicate them.
Are you really saying ordinary handhelds are a non-issue in reach them? Last I heard (not that I studied it), the CDC was putting a fair amount of effort into that (un?)platform, and getting some results.
Otoh, I grant that they’re also flogging Facebook and anything else they can find.
Educate please.
Matthew,
OK, it’s all dead. All over. What remains? What’s the cockroach of technology? What won’t die?
One answer might be the phone, in any & all forms. You allude to automated phone calls like Eliza’s (Alex Drane’s company). She & I have talked about how her company is actually a frontier mobile company b/c all those smartphones? They still can receive calls. And everyone knows how to listen (and most even know how to punch numbers on the keypad).
You are absolutely right that this essay is a geology lesson, not a blueprint. Thank you – it’s an essential point. My job is to provide the data about the reality of the world. Your job (and you do it well) is to give advice based on the data, to write the blueprint.
All very well and good!
But what about those of us who already have initiatives and are trying to get them off the ground, trying to make all the right moves, longing to see differences made, looking for support from the population who would benefit the most – the informed educated patient?!
Especially those of us who are doctors, surgeons, physicians – the people the e-patient should want working with the whole epatient initiative rather than against it!
Huh, Dave?
Isn’t Dave the marketing guy who now makes his living traveling the country selling his “miracle story of survival,” and book actually one of the 3% who got hurt when he mistakenly thought he only had 24 weeks to live based on an out-dated study he found online?
Wasn’t it his Harvard trained doc who found the clinical trial and treatment that saved his life and directed him to online communities of support? Didn’t Beth Israel already give patients access to some limited online views of their medical records (vs billing codes)when he was a patient there?
There is no question patients should be full members of their treatment teams but Dave is more typical of the data driven patients who show up with reams of computer print-outs and suddenly think they graduated from medical school and did a residency in oncology after spending a few hours doing an online search.
They often actually end up slowing their recovery down (Dave describes in his blog/book how he broke his repaired femur when he failed to follow his doctors recommendations) and most patients with cancer at some major Children’s hospitals are now given a prescription that tells them to stop doing online searches. (vs getting online support)
Dave can’t be faulted for not understanding the difference between billing codes and clinical notes given his lack of medical training or any experience in health IT or healthcare at all, but his knowledge deficit has been used by providers who are resistant to open up their records to patients and he seems oblivious to the damage it caused.
His difficulty understanding what he saw when he imported his billing codes is used as an example of how patients can’t understand their records. His story has been “misused” by the media to almost single handled destroy the personal health record movement (at GHealth at least).
What has changed at his health care institution to empower patients as a result of his experience? Do patients get to view their clinical notes (or just labs and radiology results) for example? He is very open about using his marketing background to brand himself as the ePatient spokesmodel but he doesn’t seem to actually speak for other patients or work for the same hospital that uses his story for viral marketing?
There are literally millions of empowered patients working in collaboration with providers and organization all across the country at places like Livestrong and Mayo that would probably be much better partners for you.
Updated 10:43 ET 9/15
Hey DS – thanks for piping up! Looks like Susannah touched a nerve, or maybe I did.
I’m guessing you might be the “Baltimore Doc” who commented recently on
Daphne Leigh Swancutt’s blogWhyDotPharma. As I said over there, I’m VERY interested in sorting out where you heard some of these things – honestly, sincerely interestedIf you’re a Johns Hopkins MD, as your email address suggests, I’m sure you’re not crazy, and honestly I’d like to sort through all these issues.
Just for the record, what I’m doing right now isn’t making much of a living … bounced checks (including the mortgage) are a regular event, so whatever you’re imagining, I really would like to sort it out.
And thanks for speaking up about whatever rumors you’ve heard. I really would like to sort it out, as I said on that blog, and come to a common view. I’d be happy to have a phone chat, “beer summit,” or whatever. Where I’m wrong about something, I’m more than happy to learn.
btw, DS, my contact info is on my site.
If the lineage of coincidences you point out about Dave is true then it stands to reason:
(1) Dave is a walking miracle.
(2) Through Dave’s “misused” story, he is defining best practices for the e-patient.
(3) You’ve validated his struggle: to speak on behalf of those less fortunate that don’t have the high-quality access of care he received.
One question I got directly after my talk was, “So how do I boil down all my content to fit on these tiny screens?”
Before I could answer, someone else in the crowd volunteered that her organization keeps “4 English PhDs” working full-time, editing copy down to the essentials so that their fleet of employees (pharmacists) don’t have to waste time reading a long missive. They get the short, well-written, to-the-point memo and go on with their work, saving the company millions (according to her – not my words).
I was grateful for someone else to pipe up with experience and advice, just like I’m grateful for people answering each other’s questions and offering their own insights here.
If I could, I’d now go back in time with Janice McCallum’s latest post in hand to answer that question about what to do about the tiny screens:
Leveraging Disruptive Powers of Mobile
http://www.healthcontentadvisors.com/2010/09/15/leveraging-disruptive-powers-of-mobile/
Dear DS,
First, let me disclose that Dave is an old friend, dating back to college days, as well as a patient at our hospital.
Now, let me say that your comments about him are, in my mind, patently offensive.
Just one example is contained in this sentence: “Dave is more typical of the data driven patients who show up with reams of computer print-outs and suddenly think they graduated from medical school.” First you mischaracterize Dave himself. Then, you insert him into a supposed group of patients.
You start by saying “Isn’t Dave the marketing guy who now makes his living traveling the country selling his “miracle story of survival,” and book.” Whether he is or is not a marketing guy, you use the term in a pejorative way. You make assumptions about Dave’s means of making a living and thereby his motivation.
I simply don’t understand why you find it necessary to disparage him to make your points.
Thanks to you, Paul Levy, for stepping in and supporting Dave.
As someone who’s been roused by Dave’s “marketing” message, I can’t help but notice how it’s echoed about online …
His “Calls to Action” emphasize empowerment, lifelong learning, finding good doctors, sharing what you know with others (even if it’s in the wee hours of the morning), and keeping a sustained focus on issues that matter.
I’m buying.
I thought that PaulLevy was exceptionally polite in his response to DS. But nothing will keep me from being far less understanding. Dave and I are known to be very critical of each other regularly. But critical certainly doesn’t mean disrespectful. Nobody can doubt that Dave feels in all his cells that he got a true calling, after surviving stage 4 renal cell carcinoma. Trying to take this away from him is almost like wanting to see him stop breathing.
I am shocked that in 2010 a doctor that seems associated with John Hopkins Kimmel Cancer Center uses a variety of pejorative terms and expressions to validate his opinion that the good patients are those who trust blindly their physicians and never engage into a meaningful conversation.
DS is either a real doctor and his online communication puts the reputation of his institution at risk, or more probably he is a troll, just here to make us angry because we believe he is a physician, someone with a hidden agenda that is opposition with what we are trying to do here, with our varied voices and opinions.
Forget for a second the clear personal insults thrown at Dave. You’ll see that the worst part of DS response is this much more general statement: “They often actually end up slowing their recovery down and most patients with cancer at some major Children’s hospitals are now given a prescription that tells them to stop doing online searches. (vs getting online support)”
This is the weirdest statement I have seen in a long time. It makes our earlier nemesis almost an angel.
So, DS, who are you?
I want to make it clear that I admire Dave and other ePatients for what they are doing. All of us visiting this site will most likely be ePatients oneday even if we are not already.
My issue is this: if you are going to represent a whole group of people motivating for change, then I think you owe it to that group to be diligent and explore all avenues that open up to you. Being ‘too BUSY’ is not an option in my opinion. It does not take long to point out contacts who do have the time and are interested, and are able to do things.
My initiative, in the opinion of patients more so than all other groups, is a brilliant one. To get it working as it is intended, like all startups, is going to need support. http://www.consentcare.net is the link for those who are interested.
So, who do I go to? My emails to Dave have not been answered.
Martin, I would welcome your efforts applied to the Society for Participatory Medicine in some way other than promoting your product.
I don’t understand this attitude, Dave! We have an idea with huge potential for many reasons that could benefit patients, and want to expose people to the idea so that we all benefit, both doctors and patients.
We have an ‘initiative’ out there which is free for doctors to use – your description of it as a ‘product’ is simply insulting and shows you haven’t bothered to explore it.
Your approach doesn’t sound ‘participatory’ at all, if you ask me! I’m wondering whether your whole society feels as you do. I’d really like to know!
Martin–there are many paths to the watering hole and you’d do well to ping us at Health 2.0 if you have a tech related start up that’s working to change the doctor-patient relationship. Dave is an advocate and does all he can, but he’s only one man, and to reach patients, doctors and everyone else you need to take multiple channels and not be offended that not every email gets answered.
Everyone,
I like to think of this blog & the discussions as a chance for people to learn new things, discuss trends, and meet new people — all in a cordial, collegial environment.
I’ve even started to think of some threads like a party. I set up a topic, invite a few people over, if it really starts rocking then more people join in and it takes on a momentum of its own (for example, see my “What’s the Point of Health 2.0?” post). That’s the spirit of DocTom (the blog’s founder) at work.
I also like to be part of a group blog because I don’t have to post every day to keep it fresh. And I learn more from the interactions between each of us who post since we are all (extremely) independent. My day job is totally different from John Grohol’s day job, Gilles Frydman’s day job, Alan Greene’s day job, Dave deBronkart’s day job, etc. etc.
We are, I think, an example of Dave Weinberger’s wonderful phrase (and title of his book): “Small Pieces Loosely Joined.” We are each a small piece of the conversation around participatory medicine and the social impact of the internet on health & health care. We are not, I fervently hope, responsible for the rise or fall of any one aspect of the impact or any one idea. I think Martin, for example, is in danger of mistaking the point entirely if he thinks any of us has the magic elixir of success.
We are all on the journey. Some people are shining light on the path. Others are scouting up ahead, taking risks by being out front. More are following, quietly watching what happens to the pioneers before they take another step (see my post “Happy Dogs in a Pile of Sticks” for more on that topic).
I welcome Martin, I welcome DS, just as I welcomed DarthMed (search for his name on this blog if you want the history there) because they represent opinions not often shared in public, out loud. They make me think (OK, yes, they also sometimes make me wonder). But that’s because I have the great privilege to be an observer in this space.
I hope we can get back to talking about the issues I raised in my remarks. I’m still quite interested in continuing the discussions begun at the Mayo Transform event around health literacy, digital literacy, the role of publishers, the role of pharma, the ROI on patient engagement, etc.
Thanks for your reply.
The person who succeeds is the person who does not give up, or who tries one time more than the other guy. In the modern health era, we cannot afford to give up on good ideas and initiatives, until there is public agreement that they won’t work.
This seems to be a great forum to debate them. So I will be back.
Hi Susannah – I thought I would cross post my article here. It summarises all my comments and many thanks for your comments too.
http://www.vivavip.com/go/e30388
Regards
Joanna Ptolomey (@chibbie)
Thanks, Joanna!
Your article gives the global perspective, which my data lacks since the Pew Internet Project focuses on the U.S.
After we exchanged views on Twitter yesterday I remembered an excellent article in the Washington Post by Cecilia Kang:
Going wireless all the way to the Web
http://www.washingtonpost.com/wp-dyn/content/article/2010/07/09/AR2010070905521.html
She captures the American scene: increased access via mobile devices, but distinct differences in what people do online depending on the size of the screen + speed of their connection. It’s a scene that was in my mind as I wrote this speech.
Here is an excerpt:
>>In the District, there are 232 hot spots. Last month, AT&T launched free Wi-Fi service in New York’s Times Square. Last week, Starbucks began offering free hot spots at every retail location in the United States.
To a degree, that’s helped Abraham Guardado, 16. He and his two brothers struggle to get enough time on computers at their neighborhood library to do homework and catch up with friends on Facebook. There are two iPods in their downtown Washington home, and they are able to perform basic Internet functions on those devices, thanks to a neighbor who has lent a wireless password for the brothers to get online. Guardado tracked down directions to a housecleaning client for his mother recently. He checks e-mail and found information for a research paper on NFL quarterback Michael Vick’s dogfighting conviction through searches on his Safari browser.
But he wasn’t able to watch a video of the statement Vick made before going to prison. And he had to go through many pages of search results, waiting patiently for each page to load on his device.
“It’s way cheaper than a computer, that’s for sure,” he said. “But you also have to have a lot more patience.”<<
I agree with the article. However, there is another dimension of access, which is unmentioned. That is, the “digital divide” that exists between rural communities without broadband access and the rest of the country. It is true that mobile technology can provide some relief here. However, there are even some remote households that can neither be reached via cable-based or by wireless technologies. This might affect disproportionally the poor and under-educated as covering “the last mile(s)” is often to be paid for by those households. Again, otherwise I agree with this blog post which adds much to the discussion.
Agreed, Ben – my first comment above was along the same lines (inequities introduced by differences in access).
I’ve not been following the idea of “rural broadbandification,” like the rural electrification of the Great Depression. Do you (or anyone) know its status?
Thanks, Ben, great point.
The FCC published a landmark report last February on the state of broadband in the U.S. Just 6% of American adults have dial-up access at home. One-third of that group lives in a rural area (a disproportionate share).
Here’s a link to the PDF:
http://hraunfoss.fcc.gov/edocs_public/attachmatch/DOC-296442A1.pdf
The author of the FCC report is John B. Horrigan, my former colleague, who wrote a report about rural broadband adoption back in 2006 which might be of interest for historical trends:
http://www.pewinternet.org/Reports/2006/Home-Broadband-Adoption-in-Rural-America.aspx
As for minority access, my colleague Aaron Smith just published a nice summary of what we’ve learned about technology trends among people of color:
http://pewinternet.org/Commentary/2010/September/Technology-Trends-Among-People-of-Color.aspx
Essentially:
Trend #1: The internet and broadband populations have become more diverse over the last decade, although key disparities do remain
Trend #2: Access to the digital world is increasingly being untethered from the desktop, and this is especially true for people of color
Trend #3: Minority internet users don’t just use the social web at higher rates, their attitudes towards these tools differ as well
Dave and Susan: thanks for your points; they are well taken. I am also very interested in the “digital divide” of hospitals that have EMRs.
accesibity must be, mobile could be. In this time companies follow in reverse force: accebility could be, mobile must be. Totally dissappointing.
(@redeskako)
Hi there, just doing some research for my Baltimore 4g site. Truly more information that you can imagine on the web. Wasn’t exactly what I was looking for, but nice site. Have a great day.