 A guest post by SPM member Marge Benham-Hutchins, PhD, RN, an assistant professor of nursing informatics at Texas Woman’s University. This is an email she sent me today, citing an online discussion of the appalling death in the Health Affairs column that Susannah Fox wrote about yesterday.
A guest post by SPM member Marge Benham-Hutchins, PhD, RN, an assistant professor of nursing informatics at Texas Woman’s University. This is an email she sent me today, citing an online discussion of the appalling death in the Health Affairs column that Susannah Fox wrote about yesterday.
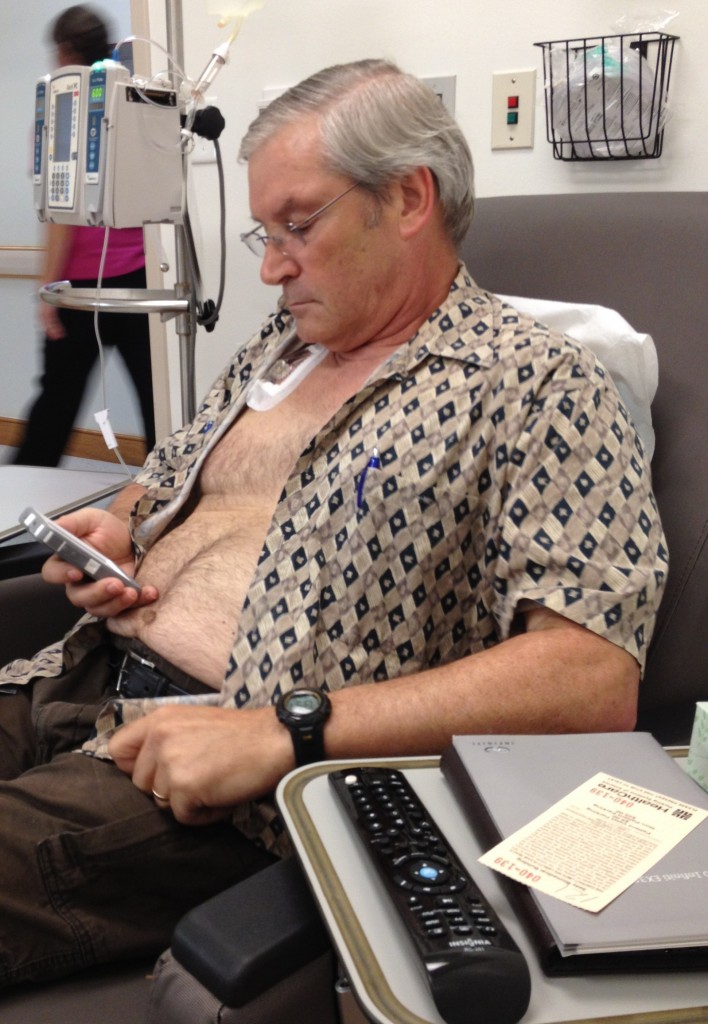
IT didn’t affect the passing of Marge’s husband from cancer [right, during chemo – “with smartphone – typical,” she says] . But she learned plenty about how far we have to go before vital information is used properly and consistently, as she shares here.
_____
Dave,
As I mentioned before I planned to work on patient and caregiver access to clinical information in the inpatient setting. The article in Health Affairs was being discussed on the AMIA nursing listserv and I posted the following. Resulted in 8 providers responding about collaborating. Want you to be aware!
_____
Hello Juliana and colleagues,
This story also hit home with me. I recently experienced my husband’s serious illnessand passing. He was in a great teaching hospital with interoperable records. Many providers used this resource to get up to date with his complex treatments, some did not and I was the source. My daughter called me the “walking, breathing, health record” and this was accurate.
Even with the tools available many providers did not use them. As a faculty member I sometimes gave them my Professor frown and asked why they had not reviewed the record. Most were shocked I asked and mumbled something about not having the time. I often pondered this phenomenon and wondered if it was time, record organization/interface or perhaps habit that resulted in providers not using the interoperable system.
A major issue I also found frustrating was that we had been using a patient portal to keep up on tests and to track results. The system had tools for identifying trends and encouraged active patient involvement. Once my husband was hospitalized the portal was no longer used for its intended purpose (nothing was posted to the portal during hospitalization) and to get copies of blood work or test results we were told to go to medical records!
Nurses were not allowed to print from the EHR but I could look over their shoulder at the screen. Oh yeah, medical records charged $20 for up to 15 pages. I was appalled and was able to get residents to print for me but this was far from the real time patient EHR access with trending we wanted.
After over a month in the hospital we moved to a rehab facility. I made the choice based on being told that they had access to the hospital EHR. I did not realize this was only the physician and it was very limited. The rest of the providers tried to piece together his history from the content in a manila envelope! I was very upset. Then I noticed something on the wall in the room, to my disbelief it was an index card for the infamous “yellow stickers” for charges!* What a nightmare!
I am very involved with the e-patient movement and strongly advocate patients as the center of care and with 24/7 access to their complete health record. This should not stop at the hospital door. As Juliana mentioned the family member and patient are important care coordinators and should be able to see the “big picture”!
Off my soapbox for now but would love to hear from others interested in doing a collaborative study on patient access to the EHR in the inpatient environment. I think a spotlight needs to be shined on this issue.
__________
Dave again … I honestly wonder:
What will it take – how much must change – before medicine evolves to bring vital information that already exists to the point of care, and have providers use it? Do some clinicians need to learn a new discipline of checking the patient’s info, because it wasn’t taught in med school?
At what point does failure to use available important information become malfeasance of some sort?
And for heaven’s sake, why not do what Planetree hospitals do: fully engage the family in using the record? At Planetree hospitals, the family doesn’t just read the record, they can write in it. It is possible, and their clinicians’ lives haven’t gone out of control.
Please: let e-patients help heal healthcare!
____________
* Re yellow stickers, Marge writes: The yellow stickers often symbolize to nurses the old paper based way of doing things. They were commonly used for patient charges. Everything from an IV kit to a bedpan had them and nurses stuck them to their uniforms as they worked and then put them on the index card or sheet in the supply room. Was not unusual to wear the darn things home!






“Nurses were not allowed to print from the EHR but I could look over their shoulder at the screen. Oh yeah, medical records charged $20 for up to 15 pages.”
That’s the money shot right there. Literally. Unfortunately, I think the issue does really just boil down to money. Hospitals are feeling pinched, so they’re resorting to the nickel-and-diming approach to sweep up some change.
Gimme My DaM Data is squaring off against Gimme My DaM Revenue. We have to lobby and deploy PR at least as well as the established players in the game – AHA and AMA as two examples there – if we’re to change that mindset.
The Society for Hospital Medicine – the professional society for hospitalists, the docs that manage care within the hospital – might be a good place to start building some collaborative muscle. I produce a podcast for SHM, and know their annual conference is in May in DC. Who wants to work with me on pitching a GMDD-themed breakout session pitch for HM13? Hospitalists are front-liners, and could be of major help, I think…
I believe there is a greater financial threat – that of litigation. It seems that some healthcare institutions and primary providers are afraid that documentation in the hands of patients and families will find the way to the lawyers office, especially when the desired outcome is not achieved. Instead of being a threat, it is my opinion that this documentation could be a way to showcase truly evidence-based, quality health care (if it existed). Even if there was an adverse outcome, the documentation can show that the healthcare team did everything right… and be proud of what they accomplished. We need to get passed the fear and paranoia and include the patient, the family, and home caregivers as part of the team with open access to records (if that is desired by these folks).
Great point – it is institutional policies developed by lawyers and backed by fear of litigation that often use HIPAA as a “reason”! HIPAA was a very different rule when developed – focus was on the portability of health insurance when you changed employers and privacy from self-insured employers from seeing your health information. Not even recognizable anymore.
Count me in!
Oops, meant to indicate that Mighty Casey could count me in!
Certainly the coming “no outcome, no income” era will impact behavior. There’s little doubt that patients/families can impact outcomes — though more data/studies would be helpful to get published in medical journals.
Taking a look at the Open Notes study left me with some clear take-aways. The biggest is that it will become the Standard of Care after it goes through the 3 stages outlined in my piece. See http://www.forbes.com/sites/davechase/2012/10/07/historic-day-in-opening-doctors-notes/ for more. The big question for me is how to accelerate those 3 stages. I hate this idea but it strikes me that some enterprising lawyers will force/accelerate this when they file class action against health systems who suppress sharing of data.
I think the ONC with Stage 3 Meaningful Use could use their bullypulpit to include Open Notes in Stage 3. Even if the outcome is they generate a heated debate (but no inclusion in Stage 3), they will have accelerated the aforementioned 3 stages of truth. My two cents to them is that the stakes are too high for them NOT to accelerate this.
I’d much rather providers use Open Notes (and similar initiatives) as an opportunity to differentiate themselves than have lawyers or the government impose their will. I think if providers don’t get ahead of this, they will find it imposed on them.
Huzzah, Dave – I agree 100%.
As I say: “At what point does failure to use available important information become malfeasance of some sort?”
Thanks Dave for helping me “shine a light” on common problems accessing clinical information by hospitalized patients.
One thing I did not mention but I believe will sound familiar to many – HIPAA. HIPAA has been used to prevent access to information – as the informed know it is not “illegal” for organizations to provide information – it is actually the opposite! I think providers and administrative support personnel need to be educated on the true meaning of this rule and to recognize they are enforcing organizational policies and interpretations of HIPAA.
My 82 year-old mother was brought to the hospital, very weak and incoherent. The hospital saw an old woman and “couldn’t find” anything wrong, so they did nothing and would not admit her. They kept saying, “she’s 82,” and kept urging us kids to come get her and sign her into a nursing home.
I argued with them over the phone, telling them to check her previous history, that she’d been through this before (dehydration). I had to tell multiple people multiple times that she had been perfectly lucid only a week before. It finally took her PCP calling the hospital to confirm that what I was saying was true.
If they had simply read her patient history, they would have seen that she’d had the exact same symptoms on her last visit to that same hospital, and responded to good nutrition and fluids. Instead, someone increased her blood pressure meds, released her to my brother, and she went home and passed out, hitting her head. She has now lost too much ground, lost her ability to live alone, lost her home and her friends.
Though I can’t prove that it would have made a difference, I believe that if the hospital had only read their own DD, or at least believed me, my mother would be in a lot better shape today.
Sharon, that’s a horrifying story. Makes me sick.
(I took the liberty of inserting some double-returns to make it easier to read online, so the impact comes through.)
I’m so sorry to hear this. I wonder what leverage we have to MAKE them do it – anyone have any ideas? There’s always suing them for avoidable harm, but I sure wish there was something people could do NOW, because I’m sure there are episodes like this happening right now.
Dave thanks so much for sharing Marge’s story. It really got me thinking about some of the topics that I have been discussing in my university class. From Marge’s story it is clear that the hospital at which her husband was cared for had an EHR system in place but were not utilizing it to its fullest capabilities to help improve patient care. There were three things that really caught my attention:
1. One of the main purposes for the switch from paper records to EHRs is to facilitate easier sharing of health records not only between physicians, but also with patients. That was why I was shocked when I read that the portal failed to update during Marge’s time in the hospital. It seems as though there should be an automatic update feature that syncs the portal with the patient’s EHR.
2. Furthermore, $20 seems like a lot for 15 pages of an EHR. The paper clearly does not cost that much. I agree with Mighty Casey. I guess that, ultimately, hospitals are businesses too, but EHRs should be able to be shared with patients through a secure interface with the click of a button. That is part of the reason why EHRs exist, so why is this feature not being employed? Then, if patients want hard copies they can print them on their own. The hospital might lose a little money but patient’s should have constant access to their EHRs.
3. Finally, the fact that the physician at the rehab facility had only a limited access to the patient’s EHR makes no sense at all. In what way would concealing some of the patient’s medical history be beneficial to the physician or for the patient? Patients and all of their physicians should have full access to their own EHRs or else patient care is clearly being impeded.
My concluding thoughts are that if we have technologies such as EHRs, why are they not being properly utilized to improve patient care? Thanks again for pointing out some of the issues that we are having with the integration of EHRs into our medical system.
Thanks for your comments! The rehab facility doctors had access based on privilages at the other hospital. So, the “EHR access” technically had nothing to do with the rehab facility. Individual doctors could access the historical record but none of the other providers could. Those providers included nurses, speech therapists, physical therapy and respiratory therapists.
I caught numerous errors by respiratory therapists as many had not been inserviced on the respiratory equipment my husband required. I was very upset by this and even had to show them how to restart the oxygen component after a power outage.
I don’t want to even imagine what would have happened if I was not there.
I was angry at times for not being allowed to be the wife – always in the nurse “protector” role.
> I caught numerous errors by respiratory therapists as many had not been inserviced on the respiratory equipment my husband required
(For those who don’t know, “inserviced” means trained, as in in-service training aka on-the-job training)
Marge, during my father’s final months at a nursing facility it was even worse – I’d find him with his oxygen canula hanging on his cheek (not in his nose) or the other end of the hose not even attached to the machine.
Patient, caregiver and provider (care circle) coordination and communication is the answer. Changing the system is taking time, healthcare’s inertia is massive.
ShareTheVisit offers mobile, HIPAA compliant care circle health care records (shared, of course) and mobile videoconferencing for virtual care circle members.
Coordination and communication, managed by the patient and their loved ones – providers welcome to participate!
Excellent post and previous comments! I think this discussion points towards an issue that modern medicine must grapple with, namely that doctors and patients utilize electronic medical records to achieve different objectives.
Patients are primarily concerned with the depiction of their condition, particularly how it relates to their perceived symptoms, and their overall well being. Patients hope that electronic medical records can convey their personal narrative of their medical condition. Doctors however, use electronic health records as a repository of patient data, meant to aid them in accurately prescribing a diagnosis and treatment for the patient. While patients hope that electronic health records will tell a medical story, doctors hope that they will point to a medical solution.
The problems that have been outlined in regards to access to medical records are challenging issues. Should every health profession in the hospital, ranging from the on-call emergency room physician, to the radiologist who images a broken leg, to the orthopedic surgeon who operates on said leg, and the anesthesiologist who places the block all have access to these records? To the layperson such as myself, the answer seems to be yes. Additionally, I find that all medical professionals, including nurses, physicians assistants, respiratory technicians, etc. should be able to obtain patient information, as I, a patient, would hope that the more information that is know about my condition, the better medical professions would be able to treat me. However, this may not be the case. The inner workings of hospitals are far more complex, with stratified responsibilities and tasks, thus making it impractical and legally unsafe to have open-access medical records.
I as a patient though, would appreciate access to electronic medical records, so that I can verify what my physician has noted, and if any symptoms were overlooked. However, I can also understand that there may be medical information in that record that I may be unable to interpret, and which my attempting to process may lead to confusion and patient discontent. Perhaps a solution to the problem of electronic medical record access would be the creation of different types of medical records, in which different levels of information were displayed, one for doctors, one for other health care professionals, and one for patients.
Hi Rohini –
> Patients hope that electronic medical records can convey their
> personal narrative of their medical condition. Doctors however,
> use electronic health records as a repository of patient data,
> meant to aid them in accurately prescribing a diagnosis and
> treatment for the patient.
I gently propose that that’s just one view, and I know plenty of patients who feel very strongly that the medical record should be a shared document, *shared* by the team (professionals, patient, family, advocates etc) who *share* the goal of the best outcome for the patient.
Each may have their own angle on that, but in participatory medicine (the focus of this blog and Society), patients are full partners and providers welcome that. (See definition at top right of this site.)
And as my own primary, Dr. Danny Sands (SPM co-founder), says, “How can patients participate if they can’t see what I see?”
Returning to the subject of this post,
> doctors hope that they will point to a medical solution.
How can that possibly happen if providers don’t LOOK at the blinkin’ record?
(Rohini, I meant to say “I know plenty of patients *and clinicians*” who feel the record should be a shared document toward a common goal.)
It is very frustrating when you cannot get access to information that you want and that would boost efficiency. Most patients want to gain a better understanding of their condition. Sometimes they need to know the inevitable consequences of their condition that were not made acutely clear in the visit to the doctor. Ultimately, the more informed patients manage their condition better, and, on average, they spend less time interacting with the doctor.
A transition from the old ways (“manila envelope”) to the new ways (EMR on your phone or tablet) will not be easy because physicians are not necessarily trained to connect with the patient through technology. As society continues to advance the capabilities of technology, medicine does too; but not with medical records. There are robots that can perform surgeries, but little can be done when a patient wants to keep track of some health information. I think this change must be introduced in medical school because by the time that clinicians are board certified, it may be too late. Doctors are very independent workers who all have their own way of accomplishing a task; even very standardized practices. It would be much easier to get physicians to incorporate their patients into the flow of information if they are taught how to do this from the beginning.
There is a wealth of technology available to the doctor to share information with the patient. The main concerns are ensuring secure data exchange, useful user interface and incentives for hospitals to provide this in the first place.
This story really struck me as an example of some of the shortcomings in the modern healthcare system that are easily avoidable. If information is there in an easily distributable form, make use of it when providing for our loved ones. There is no reason that someone shouldn’t know relevant information about a patient they are treating. It will invariably lead to one of the many provider errors that plague hospitals. This type of irresponsibility makes the numbers from the To Err is Human study, which were shocking at first, seem much more realistic.
Including us in the process could help curb these types of errors since informed loved ones often know the clinical history of the patient backwards and forwards. Patients are increasingly taking an interest in their own healthcare, as evidenced by the huge number of people that look up health information online through sources like WebMD and blogs like this one, so they will certainly be interested in the medical record as well.
Granting read-only access to medical records should be mandated, and limited writing privileges seem like a logical next step. Although concern has been raised over security, misinterpretation, and increased provider workload in studies like those by Beard et. al., I feel that these are issues that can successfully be worked around to make a necessary change that will save lives and money. Medicine is known for lagging years behind in applying technological advances, but I hope that this is one change that is made in the very near future for the sake of future patients.
Note: The Beard paper is titled “The challenges in making electronic health records
accessible to patients”
Physicians do not train for 7 to 14 years after college spending $50,000+ per year for tuition with no salary for the first 4 years and making $10 per hour working 80+ hours per week for the next 3-10 years, ending up hundreds of thousands of dollars in debt in their late 30’s with the intention of harming patients. “Do some clinicians need to learn a new discipline of checking a patient’s info” implies that it is easy to do so. Do you think physicians like angering patients by asking them a question that MAY already be documented in the chart? Have you ever looked through the chart of a complex patient? It is riddled with errors, full or relevant and irrelevant information alike and will take hours to sort through and make sense of not to mention the possibility of misunderstanding what is written by people with expertise in one area but not another. Have you played a game of telephone as a child? This is what makes the chart unreliable–the truth gets distorted and misunderstood as it is passed from one person to another. This is the nature of communication in humans. People in the field are working diligently on this problem, but it is a very complex one and cannot be explained simply by physician negligence, however much our society would like to blame physicians for everything that is wrong with health care.
So, Manu – I understand all that, and I know nobody goes through medical school to do anything less than be a doctor and do good!
The question it still leaves us with – and please try to hear this – is:
Why, then, do clinicians so often disregard the patient and family’s ENGAGEMENT with the record, when they want to check on things (as described in this post) and sometimes POINT OUT the mistakes that, as you said, are sure to be in there?
And, in many cases (which I’ve experienced, as have many others I know), why is there resistance to fixing the mistakes?
What intrigues and mystifies me about this issue is that those same people who are motivated and trained to cure will turn around and reject efforts to help, even denying that anything could be wrong in the record.
We aren’t complainers here – we’re constantly looking for what could be said that would make any difference – but on this point, years of posts and discussions on this point (here and around America) have still left us with resistance to letting patients see their data. Hence, the title of this post.
I don’t understand why physicians always sound like they’re victims when explaining their perspectives on this issue. I wonder what could solve this problem – as no one disputes what you’re saying but would like a better solution than “that’s just the way it has to be”. Are physicians actively engaged in fixing this problem? If so, who are they? Or are they passively waiting for someone else (administrators? IT companies? payers? government?) to fix this and they will work with it when it’s delivered?
Hi, SR – I know of plenty of clinicians (docs and nurses alike) who are actively involved in trying to push through the horrific usability issues of most EMRs (really REALLY poorly designed to be usable in a real-world clinical environment, I’m told) and make it all work, which of course requires that the data be accurate.
In my experience it’s hard sometimes to tease apart the many factors in a swirling mess like this. I remember the 1980s when many industries first computerized and people were forced to use CRAPPY hard-to-use systems; well justified complaints were widespread. In some cases it took a long time for usability to improve.
Here we are a full generation later (30 years) and finally medicine is starting their cycle – only because ARRA/HITCH and ONC and Medicare put gun$ to their heads. It’s completely appropriate IMO for government to have forced this industry to modernize, but we had no choice but to start with the available tools (crappy, hard to use); and now it’s entirely appropriate for the users to scream bloody murder and demand systems that don’t suck.
For some of our early coverage of these issues, see What to do about the “cream of the crap”? (Feb 2010) and “Over My Dead Body”: Why System Usability Matters (June 2010).
As someone who’s worked in software (in marketing) for decades, I was honestly shocked when I watched the Grand Rounds lecture delivered by Dr. Ross Koppel just three years ago this week. It’s linked in the February post.