 Funny how a complex cultural discussion can get triggered by something as simple as a coffee mug.
Funny how a complex cultural discussion can get triggered by something as simple as a coffee mug.
In our work to change healthcare’s beliefs about the patient-clinician relationship, nothing has had greater impact in less time than our post two weeks ago The truth about that “your Googling and my medical degree” mug. In one week it became one of our most-commented posts ever; it has 3,500 Facebook mentions and hundreds of Twitter mentions; we’ve had two follow-up posts here and here; and today, two weeks later, it’s been 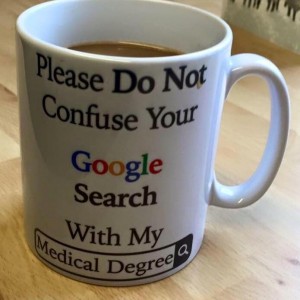 picked up and cross-posted on KevinMD, the most-read physician blog in the world, with the revised title Googling is a Sign of an Engaged Patient.
picked up and cross-posted on KevinMD, the most-read physician blog in the world, with the revised title Googling is a Sign of an Engaged Patient.
Please go engage.
I hope you will go engage in the discussion there, bringing real-world experiences.
Kevin’s blog is sometimes the scene of vitriol and reactionary complaints that boil down to “Why can’t the damned world stay the way it was when I was in medical school??” and plenty of reality-based complaints about the difficulties of being a physician (especially in the US) in an era with more and more constraints, financial and governmental. For some clinicians the reality that patient behaviors are evolving is nothing but another source of bitterness.
But not everyone feels that way, and KevinMD is a site where patients can engage in robust discussion – which we can’t, on physician-only sites.So if you want to have an effective impact on the discussion, dive in, with purpose.
In times of culture change and reality change, what works is to point to true stories, a lot of which we’ve already seen in the 74 comments on the original post. You can cross-post those or add new ones.






You won’t get 74 comments on KevinMD because, frankly, who wants to get in a pissing match with dinosaur docs in 2015.
There is no engagement possible with the commenters. We just have to wait until they are gone. And we must keep on helping patients and caregivers to instantly recognize these dinosaurs and know how to look for replacement. That’s the most constructive interaction we can have with them.
heh!
(For those who don’t know, Gilles is truly on the leading edge of all this – one of the best friends of our movement’s founder “Doc Tom” Ferguson, he’s waaaay out in front of the curve. I think he would agree that he has no use for conversations that he clarified long long ago, some of us (including me) are going along behind, persuading people year after year that the world has changed. It takes work!)
My husband has ESRD. We do hemo dialysis at home. In 2013 he had sepsis that progressed to shock. I didn’t recognize the symptoms early enough. He ended up in a coma for 5 days and had a mitral valve replacement. If I didn’t have access to an amazing nephrologist and google I would have lost my mind.
ICU staff had little hope for his survival. I educated myself and asked his dr at least 1000 questions. Sometimes the worst thing in a complicated illness is not knowing the right questions to ask. At least by googling I got enough information to be able to do that. Also was able to understand hospitals perspective. It made it easier to cope.
Scotta, that’s a wonderful addition to the many stories we’ve collected about this. Thank you!
Question: Did the doctor object to the 1,000 questions? Were you accused of thinking you’re a doctor?
Did your questions help in any way, aside from saving your sanity?
And most important, how is he now?
His nephrologist is the most gifted dr I’ve ever run into. So, no she didn’t object. We are in Montana and she was actually in Wisconson competing in a ski race but was available by cell. I probably had 100 phone calls and texts with her. She told the ICU dr.s and staff that I needed and expected all the information they could give me.
I think the ICU staff (some) and the infectious disease dr resented me. The neurologist stood at the foot of his bed while I was in the room and told me he could recover but would never leave the hospital and one of the ICU nurses told me repeatedly to make sure his affairs were in order because he wasn’t going to survive. The surgeon said he had a very small chance of surviving the mitral valve replacement.
I’m pretty sure they thought I was crazy, really. Grasping at straws.
I learned that it’s important to advocate for what you feel is right and makes sense. I made decisions about his care that ran counter to what they advised, based on what I had learned, my knowledge of him, and all the other information I received. When I argued with them they offered to move him to a different hospital. I told them there was no way in hell I was going to try and get used to a whole other batch of drs, so we were going to need to figure it out.
It took awhile (a couple days) for me to realize how sick he really was by looking everything up that they told me. If I hadn’t had google and that information to formulate the questions and his nephrologist who backed me up via long distance I truly believe he would have died. Not because of the care he was receiving, but because I would have listened to them and lost hope and took him off the ventilator etc.
It was actually 2014 that he was sick. He reminded me of that tonite. He was in and out of the hospital for about 6 mos of that year. The bacteria that landed on his heart valve essentially bathed his brain so it became the equivalent of thousands of tiny strokes. He had blood pressure that was so low at one time the neurologist thinks that he may have damaged some nerves along his spine. As a result this past year has been a climb back out of a very deep hole.
He has some residual damage to his balance and coordination and stamina. He is finally after all this time no longer anemic. We are doing home dialysis again. He is a person that is a force of nature. He was working full time as a contractor before the sepsis. The residual effect has been that he has gone on disability. He still gets up and goes to work everyday. He advises and watches and coordinates things for our son. They are/were partners before all this.
So, it’s been an adjustment. But, he is only 56. He has years and years of wisdom and experience that people look to him for, not just our family but many people in the same business. So although he isn’t physically working the way he was, he is still working and doing quite well. Staph continues to be our enemy tho. He has folliculitus now on his head, (that I also googled)
I fully agree with Gilles, it’s better to focus our energy in what is constructive rather than what is a frustrating lost battle. I too used to want to knock sense into those “dinosaur doctors” because, well, who doesn’t want to be connected to electricity or running water, right!? Wrong. Some people don’t and there is nothing that we can say to them that will make them want to see the light. As we say in French, you can’t force a donkey who is not thirsty to drink water.
A couple of years ago, frustated with doctors who have this close minded attitude I asked a professor here in Switzerland who is one of the (rare) “digital doctors” how he thought I should interact with these “dinosaures doctors” and his answer changed the way I tackle the topic. He asked me why I bother with those types of professionals instead of looking for the ones that are willing to constructively move forward alongside patients. He then added that like any paradigm change, natural selection will take it’s course, and we need those moving things forward to focus their energy on… going forward. At first I thought it was harsh, but I realised that he was right: those who do not want to “get it” just won’t, no matter how hard you want to knock some sense into them. That’s how I made the decision to leave my paternalistic close-minded oncologist (to whom I offered “Let Patients Help” as a Christmas present, and he never even read it, pretexting that he was just too busy…) I tried, it didn’t work, so I moved on. My life depended on it as we would later find out that he missed my 2nd breast cancer relapse, partly because he wouldn’t listen to my patient community knowledge information, but that’s another story. I cut my losses and went to where I would be heard and partnered with.