 SPM member Danny van Leeuwen is @HealthHats on Twitter.
SPM member Danny van Leeuwen is @HealthHats on Twitter.
Last week I attended the American Academy of Communication in Healthcare (AACH) Conference in New Haven – 2016 ENRICH Healthcare Communication Course and Research Forum at Yale, entitled, Diverse Voices, Common Vision: Fostering Effective Healthcare Communication through Inclusion.
The AACH is the professional home for all committed to improving communication and relationships in healthcare. About 200 people attended from US, Canada, Israel, Brazil, Belgium, Australia. Although most attendees were physicians, I met nurses, therapists, coaches, office managers, patients, sociologists, medical students, and researchers. A couple of very low-key sponsors but no vendors present. A pleasant relief.
The conference was designed to maximize interaction, learn from each other, and build skills within work groups and special interest groups. Met several venerable experts. Very open and quite humble: “We have a lot to learn. Especially about patient centeredness.”
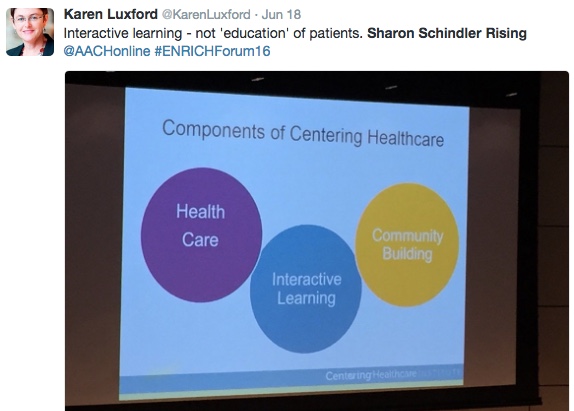
Most exciting for me was a presentation by Sharon Schindler Rising, a nurse midwife, talking about Centering Groups – facilitated groups of 6-10 young moms/couples preparing for the impending birth of a child. A wonderful example of people-centered design with participants directing much of the flow of the monthly small groups.
Professionals and services came to each group rather than each individual going to every professional and service. Groups often kept meeting on their own after the children reach one-year-old, sometimes for 8-10 years. New groups have been starting for decades. Evidence over that time showed significant increase in proportion of pregnancies going to full term and decrease in the proportion of low birth weight babies.
One sad piece of the presentation was the description of the barrier caused by the advent of the electronic health record. One participant-generated practice had been for moms and dads to enter their own health data into the paper record: instant empowerment! Not so with electronic record. People could no longer enter their own data into the health record. Shadow (paper) records had to be created. Lord, I was crushed when I heard this.
I participated in several subsequent discussions about the infrastructure and skill set that would be needed to spread the Centering Group model to other settings. Instant learning!!
I learned a new word, intersectionality (the interconnected nature of social categorizations such as race, class, and gender as they apply to a given individual or group). I took this to mean that we each do not fit into one category. We are multidimensional. Hence my brand and Twitter handle Health Hats: patient, caregiver, nurse, informaticist, leader, Opa, musician.
I attended a session about end-of-life conversations. I’m curious to learn more about AACH’s studies about that.
I found some discussion of the ecosystem (the context) of communication. Much about workforce, learning, work flow and life flow, less about technology, and almost nothing about governance. When attendees spoke of communication it was mostly between clinician and patient in hospitals and doctors’ offices and little about transitions in the community or home, and none about communication between professionals. Yet when I brought these up, there was much interest.
While I met no one working or conducting research in mental health or substance use, I did meet several people supporting individuals with cognitive disabilities of all ages. I loved the eagerness of everyone I met to discover the expertise and passion of their neighbor, to begin brainstorming how expertise could be cross fertilized, and considerable support for the hard work of effective communication. Openness, curiosity, appreciation, growth.
I was the only one wearing a Walking Gallery jacket.
The Society for Participatory Medicine and AACH have much in common – both organizations in discovery mode to continually improve communication between health team members. Quite exciting.







As Dave speaks of the “intersectionality” of the work above, and how the intersections of lives and groups enhance both, I offer the recent connection motivated by Dave. He and I share the experience of having had Stage IV kidney cancer, and that has sent the two of us off in officially different directions, all under the ‘needs of the patients”. He recently was in Calif for a meeting of the California Coalition for Compassionate Care, whose mission is to expand both palliative and hosptice care. I have been able to connect another kidney cancer patient, still living with the disease, whose interest in education has brought him to a new carreer as a chaplain. Both this patient and the head of the Calif Compassionate Care group are now connected.
Other ‘tie ins and tying ins’ to be reported from SPM members…? I know you do it also, so please let us know about how our participatory approach is linking like-minded people.
Hi Peggy – I don’t know why WordPress keeps thinking you’ve never commented here before, so it holds your comments for approval! Gr. (Plus, it took almost 24 hours to notify me of the pending comment.
For the record, Danny’s the one who spoke of the “intersectionality” – this is his post, not mine.
Thank you for pointing to the CCCC example! (And for the record there, it was SPM member Liz Salmi who made *that* connection.) Did you know they just had their first meeting of their new e-patient advisory board??