Guest post by SPM member Mark Sullivan, MD, PhD, who is Co-Director of Behavioral Health Services at the University of WashingtonCenter for Pain Relief. We welcome guest posts from SPM members – see guidelines here.
 I joined the Society for Participatory Medicine because I believe patient participation is the only path forward for medicine. We live in an era of chronic illnesses like diabetes and chronic pain, when the patient must be the primary caregiver. The average person with diabetes spends a few hours a year in front of a doctor and thousands of hours providing self-care for her condition.
I joined the Society for Participatory Medicine because I believe patient participation is the only path forward for medicine. We live in an era of chronic illnesses like diabetes and chronic pain, when the patient must be the primary caregiver. The average person with diabetes spends a few hours a year in front of a doctor and thousands of hours providing self-care for her condition.
How do we promote patient participation in health and health care? The most common answer is that we must provide patients with information. Bioethics reminds us that patients need adequate information before patients can provide consent to care. The Patient-Centered Outcomes Research Institute strives to provide the most rigorous and complete information on the comparative effectiveness of clinical treatments so that patients can make informed decisions about these. More recently, the OpenNotes movement has strived to make the electronic health record available to patients so they can understand and influence what is being said about themselves in their medical charts.
These are important steps. But patient participation in health and health care can go far beyond this. Patients can not only help choose treatments, they can help define the clinical problem to be addressed. Medical diagnosis by physicians helps link pathophysiology and prognostic information, and can point toward effective therapy. But diagnosis usually omits the patient’s experience of the illness, including both symptoms and functional impairments. Most importantly, it bypasses the patient’s perspective in its characterization of the clinical problem to be addressed. Is this clinical problem important to the patient’s quality of life? The diagnosis does not tell us this.
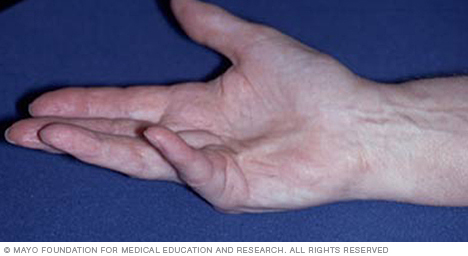
For instance, progressive contractures of the flexor tendons in the hand (Dupuytren’s contractures) may be unimportant for a lawyer, but devastating for a violinist. These get the same diagnosis, but they are not the same clinical problem.
Diagnosis in modern allopathic medicine is an impersonal process. This is its great strength and its great weakness. Any kind of person, rich or poor, saint or sinner, can have Dupuytren’s contractures. We have separated diagnosis from biography, separated who you are from what disease you have. This has made diagnosis flexible and universal. But in making diagnosis impersonal, we have separated it from the person who has the disease, who experiences its symptoms, and suffers the limitations it imposes. The personal perspective is reintroduced at the moment of treatment choice, when bioethics tells us that both medical facts and personal values become relevant to medical decision making.
But this is too late to introduce the personal perspective of the patient. It is not just treatment choices that are personal. Clinical problems are personal too. The nature of these problems, the course of these problems through a patient’s life, and above all, the meaning of these problems is personal. For care to be aligned with this very personal clinical problem, the problem needs to be defined in a personal way.
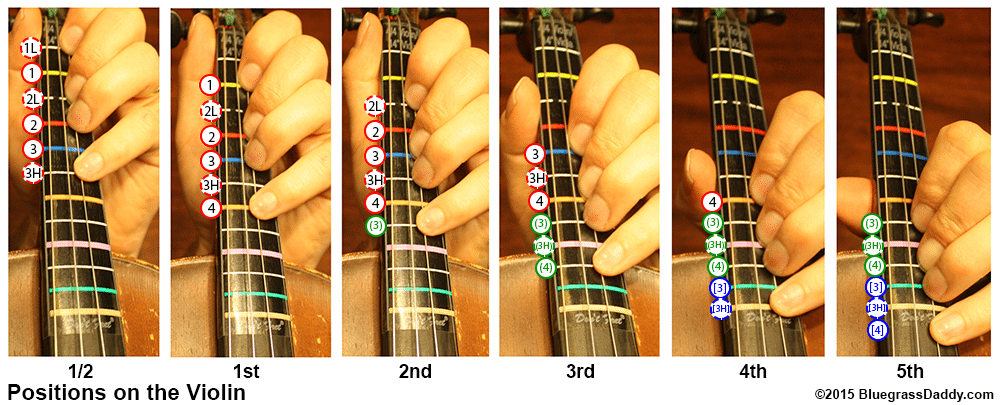
The violinist with Dupuytren’s contractures can no longer get into third position on the violin. Soon he will not be able to get into second position and then he will no longer be able to play and support his family. The lawyer with Dupuytren’s barely notices some difficulty fully extending his fingers on his left hand. He seeks diagnosis out of curiosity and seeks only prognostic information and reassurance. The violinist seeks a way to save his career and livelihood.
The patient must participate in the definition of the clinical problem. To exclude patient participation at this phase of care is to deny the authority and relevance of the patient’s perspective on his problem. Are the current symptoms the core difficulty, or are the future implications of the illness more important? Are risky treatments worth considering? The patient and clinician should form a partnership of care around an illness defined collaboratively between them. The objective diagnosis of the clinician is valuable, but so is the personal perspective of the patient. Each should have authority within the clinical encounter. Helping define the clinical problem is an essential form of patient participation in health care.
There are other essential forms of patient participation in health care: becoming an autonomous self-manager of chronic illness, becoming someone capable of carving his own environmental niche in the world, and reclaiming the authority to determine whether you are healthy or ill from the medical-industrial complex. But I will leave these for another blog post. More information about these is available in my book, The Patient As Agent of Health and Health Care (Oxford 2017) or at markdsullivan.org.
A nine minute interview with Dr. Sullivan about the book is on YouTube.
One of the earliest posts on this blog, May 2009, had a related theme. Check it out if you’re interested. Sample quote: “To alienate patients from their own decision making is to change them into objects” …. but I’ll guarantee you’ll be surprised at the source.






I am so pleased and relieved to hear of this work and emphasis on patient participation in their own input to medical involvement in their own situation. I would like to know more. I am a retired 70 year old Research Psychologist. I have struggled for years with the way in which patient involvement in their own health has been largely regarded by many clinicians, as none of our damn business. I suffer from multiple serious diagnoses of both mental and physical. I have recently been referred for Palliative care, simply because most medics have either caused some of my problems or exacerbated them by incompetence, and patronising attitudes towards me, especially when I try to obtain information from them. I have such a lot to say on this whole issue.