In the interest of speed, this is a quick note for interested parties – apologies for minimal explanation. 90 minutes from now, 2:30 pm ET on Friday 4/27, at the Health Datapalooza conference in DC, people will gather in an “unconference” session to discuss the US Veterans Administration “Open API Pledge,” which was announced last month at the huge HIMSS conference.
This is a BIG DEAL for the patient data access movement. A number of factors seem to be coming together, creating what seems to be unprecedented momentum for healthcare providers to make patient data available through APIs (software interfaces) so that app developers can collect it and turn it into more useful things. Yesterday SPM’s Executive Committee voted to endorse the pledge project – SPM and its members have been advocating for this for years. The current project doesn’t provide unlimited access but includes far greater access than anything before – and, importantly, far more agreement to participate.
Recent history:
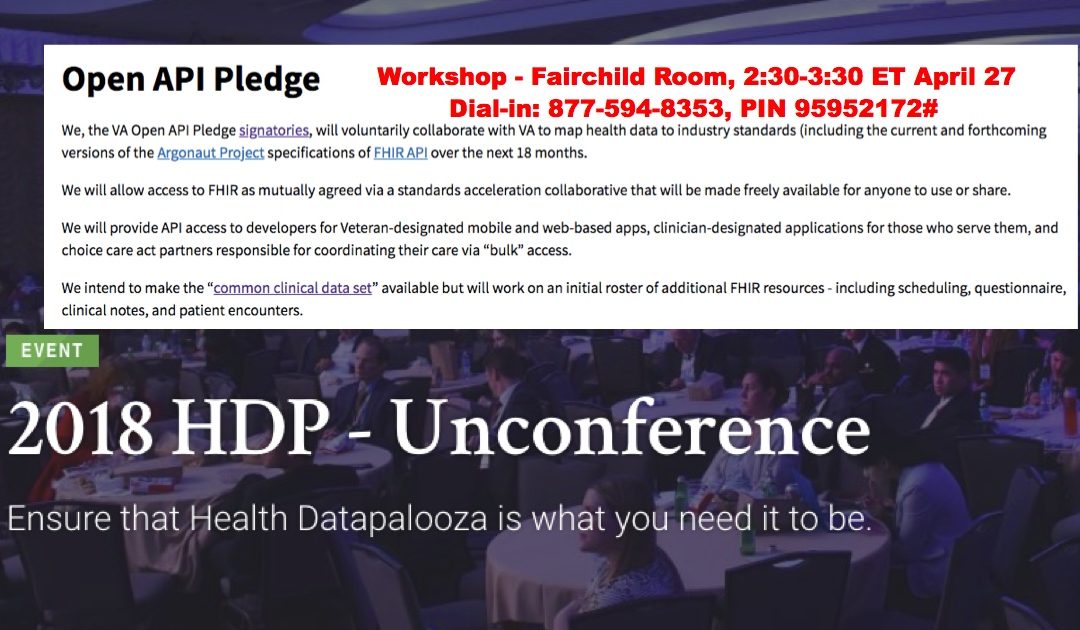
- The pledge wording is in the graphic above, and is here.
- On the last day of HIMSS (last month), VA then-Secretary Steve Shulkin announced that the Pledge project will be led by Rasu Shrestha MD, head of innovation at UPMC (University of Pittsburgh Medical Center). At the time eleven high-profile healthcare provider organizations signed on – Hopkins, Mayo, Partners (Mass General et al), Beth Israel Deaconess, etc. (Full list is on that link.) Since then the list has grown to >170 signers. (They’re not yet listed on the site.)
The 4/27 meeting:
This was an ad hoc gathering of interested parties to discuss what’s next. In an email yesterday Rasu shared this agenda:
We will have an in-person meeting at the Health Datapalooza in Washington DC on Friday (April 27; 2:30 PM – 3:30 PM EST; Location: Fairchild Room/ Terrace Level) where we will talk through the following items:
- OpenAPI Pledge – where are we, and where are we headed
- What should a charter look like
- Breakdown on OpenAPI pledgees – and what’s next
- Working group details + housekeeping items
- Slack
- GitHub
- Planning around communications/ press releases/ newsletter/ communication calendar tied to action points
- VA Lighthouse update
- Open Q&A / Townhall style discussion
Anyone is welcome to attend in person or dial in: 877-594-8353, PIN 95952172#
=================
Live blogging notes during meeting
Captured by SPM member Casey Quinlan, Datapalooza committee member; posted here by Dave deBronkart:
- Rasu opens. No rules, unconference. OpenAPI pledge. Distributes a handout, which will be emailed to you.
- HIMSS closing keynote, Shulkin, mentions OpenAPI Pledge starting up.
- Talks about link shared above. 170 signatories on Pledge so far.
- Challenges of interop; instances of Cerner and Epic, trying to get them to talk to each other
- At VA, which was Epic and now moving to Cerner, air of uncertainty currently due to VA Director gig being unfilled at the moment.
- At UPMC, belief is that when systems were first implemented, they were implemented as silos.
- To make care coordination real, data must flow freely.
- VA is largest health system in the country. $10B contract w/Cerner = HUGE opportunity, 1ce in a lifetime, to rally around and use it to make something BE interoperable, and show the way to the rest of the healthcare landscape on how to do it.
- VA is largest health system in the country. $10B contract w/Cerner = HUGE opportunity, 1ce in a lifetime, to rally around and use it to make something BE interoperable, and show the way to the rest of the healthcare landscape on how to do it.
- Leaders in EHR major players, when you say “open up, you’re a closed system, be interoperable” answer is “we’re as open as we need to be.” Shifting focus to “I’m a customer, and this is what I need, here are the use cases” (HL7, FHIR, et al), collective ask by customers w/one unified voice, the vendors have started leaning in.
Bill James, acting Deputy CIO of the VA:
- My focus, my clarifying perspective, is that it’s all about the vets. How do I help a vet use his/her own data to enhance their wellbeing and health?
- Big data, sure, but the clarifying question is “how does this help a veteran?”
- That focus will pull us through the challenge to make interop real/real useful.
- Have spent half my career in govt, half in private sector. Govt regs on doing business with feds are arduous. Micropurchases via API pledge can be a lever to accelerate progress without bogging down in federal procurement process.
- Makes analogy to ATT breakup in ’82.
- Aneesh Chopra: Chris at Mayo, take it away
Chris/Mayo:
- Comments made so far are on point. Mayo wants to serve veterans well, return all care data to VA easily to make care process frictionless. We see it as “and” not “or”. Access rules and consent rules need tuning, but that’s doable
- Standards and tech will help facilitate.
Shavik:
- One of the things that I’d ask is that we recognize veterans are still serving in being part of this effort. Care that happens in VA and in community can be done together, well, through this effort. Interop means more data for research, too. Improve science of care coordination in addition to better individual care.
Rasu:
- Vision: Partner with health-sector leaders and other government agencies to open data models by establishing data standards and open data sharing through APIs.
- Reads the pledge. Notes: this is not intended to be competitive with other FHIR and Argonaut projects, Rather, provide a level of focus, intent, and purpose that hasn’t existed. To say all that is wonderful; here are specific things we think we would need to push the veteran agenda forward.
- Intent: Encourage health organizations to open up their health data models (EHRs, pharmacy, research, etc.) and enable open sharing across systems.
- Outcome: Patient centered transparent data sharing for all patients as they interact with health organizations – from initial contact to appointment with provider to ancillary follow up actions.
- We, the VA Open API Pledge signatories, will voluntarily collaborate with VA to map health data to industry standards (including the current and forthcoming versions of the Argonaut Project specifications of FHIR API over the next 18 months.
- We will allow access to FHIR as mutually agreed via a standards acceleration collaborative that will be made freely available for anyone to use or share.
- We will provide API access to developers for Veteran-designated mobile and web-based apps, clinician-designated applications for those who serve them, and choice care act partners responsible for coordinating their care via “bulk” access.
- We intend to make the “common clinical data set” available but will work on an initial roster of additional FHIR resources – including scheduling, questionnaire, clinical notes, and patient encounters.
- Rasu: not just talking about DOD/VA interop. Choice Care Act in play too, with promise that veterans can get care in their community, from community providers. Interop THERE, too, is big part of this.
- Common clinical data set (aka USCDI): https://www.healthit.gov/sites/default/files/draft-uscdi.pdf …
- The “where we are” page (see logos): https://www.oit.va.gov/developer/pledge.cfm#signatories
- Moving outside app development, into that non-traditional vendor/partner/developer landscape.
- Rasu: spent time shadowing VA docs and talking to patients. PTSD, TBI, other injuries. Most deserving of most excellent care we can deliver. They wait forever for appointments, care, it’s difficult. They’re burdened with the cost of their service, and then burdened again with the hurdles presented by accessing care.
 Tech can streamline this. UPMC has “SingleView” – unified view of UPMC patient across many tech platforms, in one screen/dashboard. Can do this at the VA!
Tech can streamline this. UPMC has “SingleView” – unified view of UPMC patient across many tech platforms, in one screen/dashboard. Can do this at the VA!- Where we want to go: we need to get organized. Big players are leaning in, 170+ signatories. Now we need to formulate a charter.
- Signatories need categorization. Big players like Epic, Cerner, Allscripts, leaders are open in their support. Argonaut, HL7, FHIR are toolkit.
- Collective ask: scheduling, toolkits, hackathons, define/highlight early successes in workflows, transitions, etc.
- Work on charter immediately. Argonaut has good template, framework for us to use to create it.
- Resources they’re already using: a Slack channel, Github. (These may not be tools you’re accustomed to the government using!)
- Public facing & private facing workspaces.
- Communications framework: have a plan; will include newsletter.
- Spread the word by social media. Blogs, LinkedIn, posts, graphics…
- Specific activities announced on the regular.
- What we want to highlight, and when.
- Social media will be a major channel.
- Hashtag
#OpenAPIPledge will be registered w/Symplur – blonde woman here said she’d do it.
Q&A:
 Former SPM member Fred Trotter talks about experience with the DIRECT project. Certificates were a BIG problem. Certificates in VA universe is … hard. “Could we please not do that again?” Rasu: YES.
Former SPM member Fred Trotter talks about experience with the DIRECT project. Certificates were a BIG problem. Certificates in VA universe is … hard. “Could we please not do that again?” Rasu: YES.- Aneesh Chopra: opening up pledgees’ provider directories would be a good way to start to tackle this
- SPM member Josh Rubin, Kanter Family Foundation & UMich Med School: signed the pledge. Seems to be all about developers, there should be something about health data rights, statements about us/the project’s own transparency
- Here’s the Declaration of Health Data Rights written at HealthCamp 2009 in Toronto – is it what you’re talking about?
- SPM member Michael Mittleman: can we get some veteran representation on the working group on this?
- Rasu + VA rep: veterans in HDP audience this week have been giving us real time feedback.
- Rasu / Casey / Dave met Weds night & talked about “health data spigots” not trickles. Society for Participatory Medicine. (That link is Dave’s post on the GetMyHealthData site.)
- Level of engagement, SPM involvement, resonated in conversation.
- SPM member Janice Tufte: I’m a family survivor as well as a patient. Will families be included? VA rep: YES
- Use cases will be captured in real time.
- Tufte: In Washington state, veterans are leading in creating care coord in mental/physical/psychosocial health.
- VA rep: telepresence is what we’re seeing, beyond “telehealth”
- First APIs will be from Veterans Services Organizations. “Turbo Tax” type experience, work through prompted info input, get what you need to have at the end (documentation, appointments, schedule, etc.)
- @AmyEdgar: Have been working in suicide ~12 years. Let’s not forget the people who’ve become disenfranchised. Has been working on veteran suicide, outside “usual” channels outside VA. Groups outside VA are first line triage for many vets with trauma issues.
- Mittelman: hackathons – what about doing some at VFW posts? In less populated regions they’re sometimes the best gathering point.
- Casey: Richmond, VA. Big tech community, McGuire VA, Virginia Biotech Park, RVAtech (tech council), VCU Med. I volunteer to shake trees to make an OpenAPI Pledge hackathon a thing in Q4 ’18.
- VA rep: micropurchase stuff will start happening now, < $10K. That’s a nit (hardly anything for feds, but YUUUUGE help for a startup.
- Rubin: opioid epidemic, suicide are issues that transcend “health care” – where are those in this?
- VA rep: suicide/behavioral risk PHQ9 survey stuff is getting addressed using Argonaut and FHIR. Shavik: we’re working on that
- Mark Scrimshire said something about CMS, APIs, and not being known for playing well with other federal agencies. Laughter ensued.:-)






Recent Comments