SPM advocates vociferously for patient ownership of their own data. Success would be revolutionary. But revolutions do not suddenly appear. They result from persistent long-term effort, strategy, and tactics. Key milestones often only appear in hindsight. The revolution won’t happen with patients alone. The partnership with their physicians and other trusted licensed clinicians is critical. Physicians and other licensed clinicians express increased frustration – no, outrage – that the electronic health records support billing, not clinical care. See the National Academy of Medicine’s Care-Centered Clinical Documentation in the Digital Environment: Solutions to Alleviate Burnout. Could we be approaching a harmonic convergence to take data control for patients and trusted clinicians? Could a Give Me My DaM Data revolution be upon us?
For me, Give Me my DaM Data means
- Data that matters to me
- Data that I can understand
- Data that’s correct
- Data that I control
- Data I can use to make decisions with my trusted clinicians
In short: Everyone with permission from me sees the same correct, up-to-date data set.
Let’s consider #4 Data that I control:
- I can access it easily
- I can track who or what is trying to see it, actually sees it, adds to it, changes it (history of use)
- I can give and withdraw permission to whom I want
- If there’s money to be made from it, I get some of it
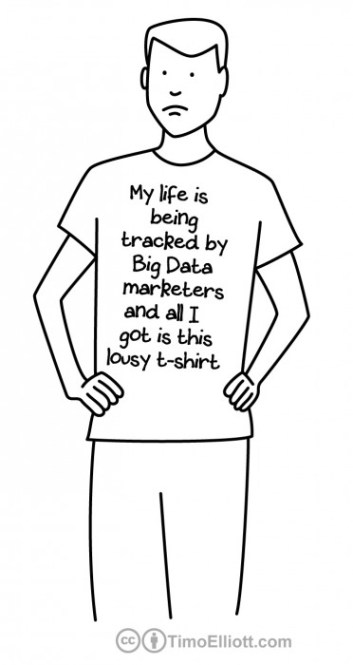
Right now, data about me is controlled by EHR and health app vendors, hospitals, insurance companies, government, and companies with a business model that sells data about me – not me.
Control becomes more difficult as I have more diagnoses, more clinicians, and settings of care, more medications and treatments, and get older (more history). Add challenges of capacity and cognition (young and old) and it gets even harder. Certainly, control has political, financial, cultural, and behavioral components. The business of health data is powerful and entrenched. Policies and inertia favor business, not people. The will to manage control for patients is weak but growing.
Paradoxically, the technology for patient control of their health data is much less challenging than will, policy, and money.
For patients, the technology needs:
- To make access to data easier for us: web-based with an authorization server (a traffic cop between all the users and creators of data and the data storage places) and work with any device as long as there is an internet connection
- To contain the right information: up-to-date medications, allergies, problems, plans, and social history with the ability to reconcile with a trusted licensed clinician
- To allow secure communication with licensed clinicians who have access
- To be able to pull data from participating hospitals, clinics, and pharmacies, and personal health apps
- To have default policies (rules and standards) set for convenience
- To have the ability to set a proxy user (care partner) in case we are unavailable or incapacitated
- To allow us to enter new /edit existing data, signed off with a trusted licensed clinician
- Dynamic client registration that allows new clients to gain access with permission from me without me needing to generate individual agreements or specialized technology for data access (client = users and contributors)
- Clinical decision support capacity
- Text or e-mail notifications for new access requests or entries to my health record
For physicians and other licensed clinicians, the technology needs:
- A single sign-on feature to connect to any number of patient health records at the same time without remembering each one
- A simple, intuitive, easy to use clinical documentation system
- To be able to synchronize patient data to a clinic-based EHR.
- Template generation on-the-fly functionality. This means automation or machine learning about repetitive technology tasks. An example: A template could be an X-ray report that contains the same headings in the same order or a common list of drugs prescribed to patients after a heart attack,
- To include growth charts, social history documentation, secure messaging with the patient, and scheduling capabilities
- The capacity to use any device to input and view a record, even from a smartphone
- A ICD-10 lookup engine from CMS (Center for Medicare and Medicaid Services)
- Medication lookup engine from RXNorm
- e-Prescribing and orders done through blockchain digital notarization process
- Tagging features for encounters (categorizes like visits)
- Basic clinical decision support (US Preventive Services Task force recommendations, CDC Immunization guidelines, HEDIS measures, GoodRX (prescription pricing comparison tool)
- Text or e-mail notifications for new entries to the patient health record
Thankfully, patient and licensed clinician interests align here. Patients and clinicians need control over our data. Physicians and other licensed clinicians are the most frequent contributors and users of that data about us. Patients are the primary carriers of that data from setting to setting over their lifetimes. The most important part of a revolution is market power for patients and licensed clinicians. Without stuff that we can actually choose and buy for ourselves, the introduction of the features listed above will be slow or nonexistent – think policy, politics, inertia, money. Market power comes from turning OFF, ALL of the institutional uses of data that do not go through a specific patient or clinician that has an actual choice. No more use of de-identified data to avoid consent. No more proprietary interfaces to avoid choice. Wresting control of tools essential to our health and well-being from those corporations. A key to that control is Open Source. Actually, medical care is already Open Source. Open Source means sharing, open exchange of ideas, learning together by doing and trying in a supportive environment. Best ideas win. What works wins. Communities form to multiply efforts and share. ePatient communities are inherently Open Source. Open source technology for Give Me My DaM Data is a natural fit. Follow SPM’s advocacy for patient ownership of data here in the Advocacy Community. I will be attending a National Academy of Medicine (NAM)’s Digital Learning Collaborative (DLC), in DC on June 28th that focuses on patient ownership of health data and the implications for a learning health system. Sessions will include discussing the vision of a health system where patients own health data, defining patient data ownership, discussing the ethical and financial implications of patient data ownership, and identifying the social, political, and regulatory changes need to accelerate responsible data ownership. Adrian Gropper leads an initiative, HIE of One, working on the technical aspects described above. What else are SPM members working on? Let’s share on the SPM Advocacy Community.






Recent Comments