Great update 20 months later: UCSF Hospital announced Jan 10, 2020 that they’ve made radiology images available through their MyChart portal, and Dr. Mark Kohli tweeted that it’s due to the speech that resulted from this blog post!
Here’s their blog post, Jan. 23, about it.
This is so exasperating. For years we at the Society for Participatory Medicine have been among the leaders of the movement for patients to have access to their medical records, in EMRs and everywhere. We’ve blogged repeatedly (and advocated in DC) about patient access to medical records and your HIPAA privacy and access rights, and we’ve been among the most vociferous advocates for the OpenNotes movement, where you get to see what your clinicians write in the computer. In every case we’ve won the argument, because everything we’ve said is just plain right (factually and ethically), and because every skeptical voice who doubted it was simply misinformed. And while we’re still beset with foot-dragging providers who resist sharing (sometimes for commercial benefit), the deniers have pretty much stopped their denial.
But now we have to start over with a faction of the healthcare industry – innovators, investors, health IT people – who have begun expressing the same doubts about our radiology images, and asking the same benighted, ignorant questions: “Why would patients want these? I wouldn’t want to see mine – that’s why I have doctors! Besides, patients aren’t radiologists – they can’t understand the images – so what would they even DO with them?”
Meanwhile, ACR, the American College of Radiology, is an association member of SPM, which suggests the profession itself has no doubt about the value of patients being well informed.
Questions like “Why would they even want them” are asked by people – perhaps well-intentioned, but uninformed – who’ve never had a problem that makes them worry about whether they, or their child, or a parent, will survive. It’s dangerous in healthcare to get advice from people who’ve never been in medical danger. Let patients help tell you what matters when everything is on the line.
(See Joe Biden’s impassioned speech two years ago about how infuriating it was to have his son Beau’s cancer treatment impeded by data mobility problems. When Epic’s Judy Faulkner later asked him scoffingly what he’d even do with his EMR data (sound familiar?) he said “None of your business!”)
Last week I gave the opening keynote at a radiology informatics conference, SIIM 2018 – the Society for Imaging Informatics in Medicine. Its theme was “Inspiring Collaboration,” and as SPM chair and co-founder Dr. Danny Sands often says, “How can patients participate if they can’t see what I see?” For examples, in preparation for the talk I asked on Facebook [image, right] whether anyone I know has a story of how having access to their radiology clearly made a difference. Wow, what responses. You can read the whole thread (some amazing tangents arose, btw), but here are my top highlights, in roughly chronological order as they came in.
Sara Riggare, Stockholm
 “10 days ago I injured a toe in a staircase, it was X-rayed last Monday and I was [simply] told I had a fracture. I asked for the images and after being persistent, I was told they would send a CD by post. It arrived last Friday and after downloading a DICOM viewer to export the images to jpg, I could show the scans to my chiropractor who gave me specific advice for selfcare that I didn’t get from the doctor.”
“10 days ago I injured a toe in a staircase, it was X-rayed last Monday and I was [simply] told I had a fracture. I asked for the images and after being persistent, I was told they would send a CD by post. It arrived last Friday and after downloading a DICOM viewer to export the images to jpg, I could show the scans to my chiropractor who gave me specific advice for selfcare that I didn’t get from the doctor.”
Seeing where the fracture was, the “chiropractor told me that I need to keep the toe taped with the next one for at least 4 weeks and wear shoes with a non-flexible sole. Also that I should try walking on it as much as I can.” I asked “that advice would not have been possible with just the finding ‘yup, it’s a fracture’?” She replied, “Correct, she first needed to know where the fracture was situated and what it looked like.”
Liz Salmi
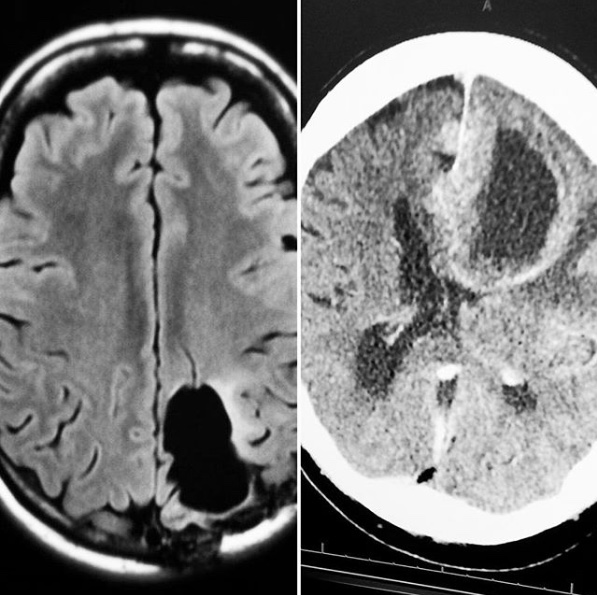 “I crowdsourced a glioblastoma diagnosis for my dad through Twitter using images from a CT scan [right – her “family portrait” – her own brain tumor on the left, Dad on the right]. He had a pacemaker and couldn’t have an MRI. He refused treatment so we couldn’t get tissue to confirm pathology. But the image was textbook glioblastoma. Neuro-radiologists on Twitter weighed in (conservatively) to help us make decisions. Results: 95% sure it was GBM, 5% chance there could be a weird brain infection.”
“I crowdsourced a glioblastoma diagnosis for my dad through Twitter using images from a CT scan [right – her “family portrait” – her own brain tumor on the left, Dad on the right]. He had a pacemaker and couldn’t have an MRI. He refused treatment so we couldn’t get tissue to confirm pathology. But the image was textbook glioblastoma. Neuro-radiologists on Twitter weighed in (conservatively) to help us make decisions. Results: 95% sure it was GBM, 5% chance there could be a weird brain infection.”
I replied noting that some skeptics will always say “But did that make any difference??” The question belies the unspoken assumption – by the ignorant – that radiology only involves yes-no questions in nice clear-cut situations. Liz’s answer: “My dad had expressive aphasia, couldn’t speak (though could understand), and was falling and having seizures. He didn’t want to prolong things. So knowing it was glioblastoma vs. a random infection was important.”
What a poignant illustration of how wrong it is to ask whether the informal diagnosis made any difference. It illustrates how just plain benighted it is to say “You can’t have your images unless you give me a reason that I think is valid”: it’s our data, and you have no idea what value we may find in it.
Amy Price
“I used them to tailor brain rehab. The neuroradiologist explained them. I also used them to change behavior. For the spine, SDM [shared decision making] and co-design of treatment. I looked at the places that were damaged and analyzed their function, That gave me an objective picture of how it influenced behavior; when I knew it was damage and not me I was able to change my behavior and actions and not feel ashamed. It has also helped with several other patients who all had the same experience, in this case knowledge was power!”
Claire Snyman
“For me, having my own images was life saving. As a brain tumor patient, I got acutely ill with migraines, vertigo – was misdiagnosed – my brain tumor had actually doubled in size – I had hydrocephalus. This was confirmed when I finally got a private pay MRI (I live in Canada). I asked for a CD copy of my MRI and was able to upload my images to my second opinion at Johns Hopkins. He was able to view my MRI, recommend immediate course of action – which involved me flying to the US next day. Straight into ICU. I have copies of every MRI/CT scan of mine.:-)”
Amy Morrison Regenstreif
“I learned how to read my images… and reports … many times over 16 years rib tumors were missed … I found them.
“Medical folks that don’t teach patients or try not to pass on records have egos way too big ….” Posted later on the SPM FB page
Tim Kroesbergen
“Two summers ago I went on holiday in France. In an accident I broke two of my legs. When I got an x-ray in a local hospital I photographed those x-rays and sent them to my doctor in Holland. The next day I was able to travel back to Holland where I live and was operated one day later because they had those messaged x-rays so they could prepare.
“By sending over my French x-rays they could speed up the process, give me better advice (as the doctors in Holland know about my disease, the French did not + communication was difficult) and plan a sooner operation in Holland.”
Kelly Young (@RAWarrior)
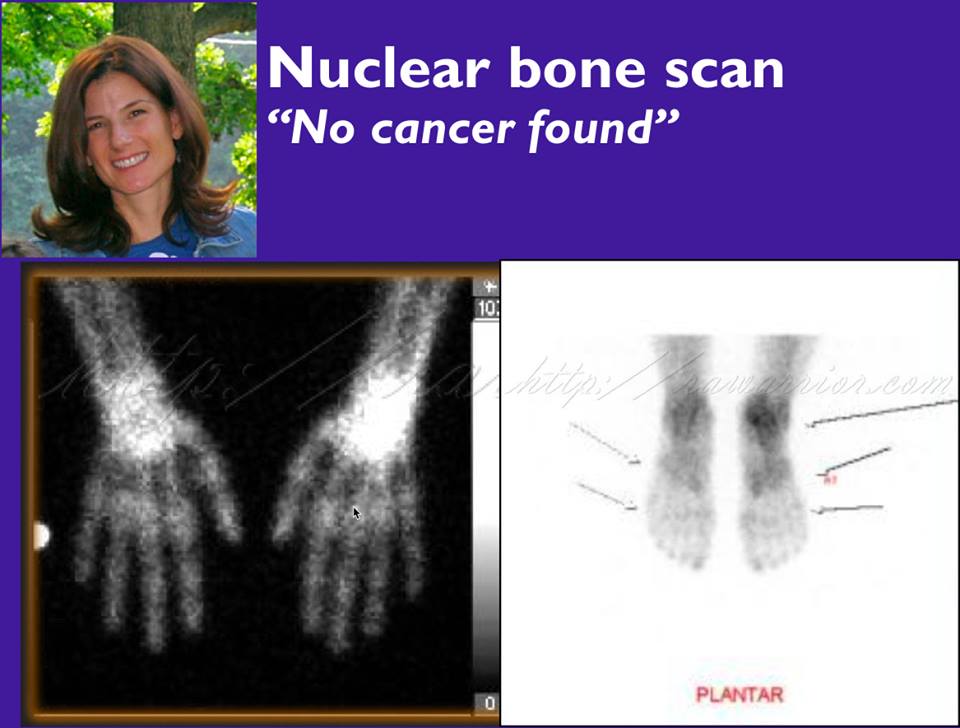 I must also mention Kelly, who was the last patient story I told in my TED Talk. She’d gotten a nuclear bone scan, which is usually used to look for cancer but in her case was looking for “hot spots” of inflammation. Somehow the radiologist ignored the indication (the problem they were looking for) and inappropriately said “no cancer found.” She got the images and saw the hot spots, indicating the inflammation that her doc had been denying.
I must also mention Kelly, who was the last patient story I told in my TED Talk. She’d gotten a nuclear bone scan, which is usually used to look for cancer but in her case was looking for “hot spots” of inflammation. Somehow the radiologist ignored the indication (the problem they were looking for) and inappropriately said “no cancer found.” She got the images and saw the hot spots, indicating the inflammation that her doc had been denying.
The stories above all involve the patient having access to the image data, but another story on the thread showed real value just from having access to the written radiology reports:
Danielle Achs Edges
“I can’t say on images – but I can say on radiological reports. I found a very crucial missed issue on [my daughter’s] liver ultrasound radiological reports for a 2 year period done every 3 months. Completely changed the course of her care.
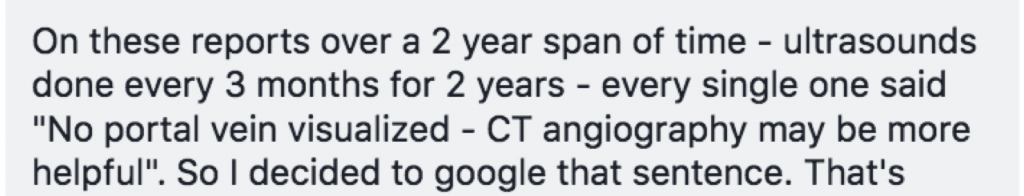 “Every single one said “No portal vein visualized – CT angiography may be more helpful”. So I decided to google that sentence. That’s when I fell down the rabbit hole and discovered this rare condition called Abernethy Malformation (congenital absence of the portal vein) and the complications it can bring which fit my daughter’s complications perfectly. So I called the hepatologist and said we need a CT with contrast stat (of course gave him all the med journals I read about it) and 2 days later we had confirmation of Abernethy Malformation.”
“Every single one said “No portal vein visualized – CT angiography may be more helpful”. So I decided to google that sentence. That’s when I fell down the rabbit hole and discovered this rare condition called Abernethy Malformation (congenital absence of the portal vein) and the complications it can bring which fit my daughter’s complications perfectly. So I called the hepatologist and said we need a CT with contrast stat (of course gave him all the med journals I read about it) and 2 days later we had confirmation of Abernethy Malformation.”
ACR resources
As noted above, the American College of Radiology is an enthusiastic association member of our Society for Participatory Medicine, which as the name implies is about patient-clinician partnership. On this Facebook thread the ACR’s Becky Haines posted two relevant resources that further address the “What would a patient do with it?”
- “If you all are looking for patient-friendly radiology info, it’s here: www.radiologyinfo.org“
- “Also the work on getting access to the Imaging Appropriateness evidence base here: https://www.jacr.org/content/ac-patient-summaries Written by patients!”
Again, these are only some of the anecdotes shared on that thread. If you read the whole thing (including sub-comments) you can see how many people have either improved outcomes by being informed and engaged, or have had the system fall short of its potential.
Parting thoughts from medical leaders
Our thinking above is not new, but beliefs and paradigms change slowly. All snark aside, please remember: leading physicians like Warner Slack (“patients are the most under-utilized resource”) and Tom Delbanco (OpenNotes, Healthcare in a Land Called PeoplePower) have spoken since the last century of patient power enabled by data. Similarly, our society was founded by friends of “Doc Tom” Ferguson, who first documented e-patients in the BMJ in 2004, saying:
The emerging world of the e-patient cannot be fully understood and appreciated in the context of pre-internet medical constructs.
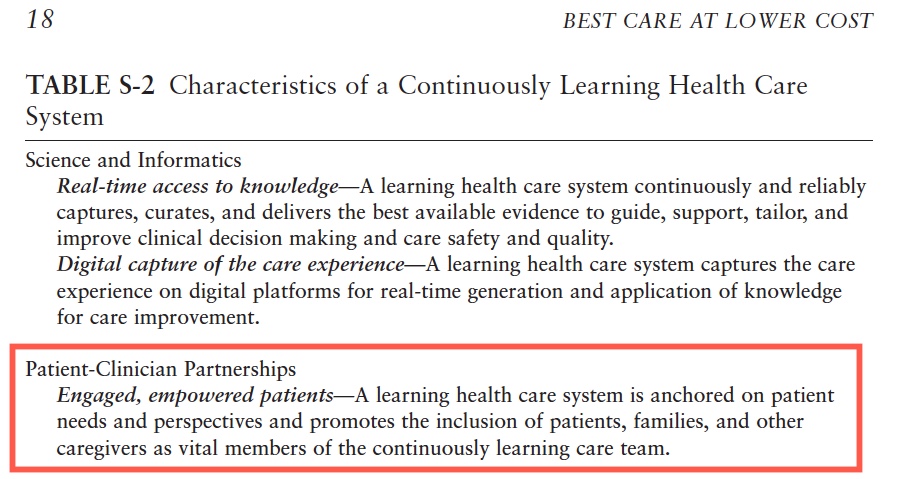
That was before the first smartphone, and before the iPad and other tablets and nearly ubiquitous wifi changed the presence of data in our lives – and the expectation of holding our data in our hands. Then in 2012, in Best Care at Lower Cost, the Institute of Medicine wrote (Table S-2) that one of the four cornerstones of the future of healthcare was (their exact words) “Patient-clinician partnerships” with “Engaged, empowered patients.”
Think again about Dr. Slack’s remark – as far back as the1970s – that patients are the most underused resource in healthcare. Please don’t perpetuate that by limiting patient access to case information. In everything you do and design for the future of healthcare, please err on the side of letting patients contribute to the future of care.
And a PS from the inventor of the Web
In that same TED Talk I recounted how Tim Berners-Lee himself – inventor of the Web – spoke at TED2009 and told the audience:
“…give us the unadulterated data, we want the data. We want unadulterated data.
OK, we have to ask for raw data now. And I’m going to ask you to practice that, OK? Can you say “raw”? [“Raw!’] Can you say “data”? [“Data!”] Can you say “now”? [“Now!”] Alright, “raw data now”! “Raw data now!’]
Practice that. It’s important because you have no idea the number of excuses people come up with to hang onto their data [the data they were paid to generate] and not give it to you,






I have what might be a slightly different angle on this issue: I was a caregiver for an elderly man with various orthopedic problems left over from a 65-foot fall when he was 18. Over 10 years, we moved several times and changed doctors because of that. Having his images and radiology reports have saved time, money, and discomfort by enabling his new doctor to see what he’s dealing with without requiring the same battery of tests each time.
Also, I have been able to use previous images to short-circuit irrelevant diagnoses for symptoms that I know to be related solely to his old injuries. On the other hand, when this man has had to go to the ER for something and I couldn’t be there, NOT having these images and records in his EMR has resulted in unnecessary testing AND distraction from the acute problem that he was having as the doctors got caught up in reviewing his old injuries.
And don’t get me started on med lists! If he ever went to a particular hospital, they have THEIR version of his medlist from that previous visit, which might be years ago, but no information about his CURRENT list, which is often quite different. If they won’t give me access to the doctor in charge, I am never sure if they are working off the old list or the new and have to watch like a hawk to make sure he is getting everything he needs and nothing he doesn’t need. The EMR should be a SINGLE database that all hospitals have access to!
Excellent added examples, Nora – thank you!
Re the med list etc – it’s so easy to prove, as you did, that lack of that single record causes harm and expense. The reality is that every provider has his/her/its own system, originally designed for their billing, and it’s highly unlikely those will ever get mooshed together.
That’s why I personally believe in a health data spigot to let us get our data OUT of those malformed systems, and into something truly oriented around you and your needs.
I think that I could have saved my child from a preventable adverse event, if I had only been able to get all the medical records immediately. (sigh)
Emily, I’m not able to view that YouTube – can you say something more specifically about access to radiology images?
My child fell in our garage and had 2 radiology reports for a right arm injury. The 1st report indicated 3 fractures in the right arm.(Unfortunately,I didn’t get this 1st radiology report for well over 6 months, & I was shocked to learn that there were many fractures.) The second report indicated only one right arm fracture, and my child had a closed surgery, 8 days after injury based on only one fracture. My child now has uncorrectable -05 pronation, 40% subluxation and post traumatic radioulnar synostosis. Over time, I’ve found additional medical record errors: dates, history of treatment, type of surgery, omissions etc. I feel bad that I couldn’t see medical records on day one and get things corrected. Other families need their records!
Thank you, Emily. That’s terrible. You’re right, if you’d had full access it seems pretty clear that significant trouble could have been avoided. Thank you for spreading the word.
I just donated, and it felt great. Thank you to the “Society for Participatory Medicine.” I originally heard about you in Facebook group “Mothers Against Medical Errors.” Families are sharing radiology and medical records with each other already, but it’s sometimes done to just figure out harm. What I love is the future-oriented, affordable aspect of this plan, putting patients and providers on the same team from the get-go. If just 1% of families avoid harm, imagine the physical, emotional and financial savings. Win-Win!
I had a breast cancer scare a few years ago at age 19 (it was benign). I was pushed doctor to doctor in a small town until I got to a radiologist. Because the radiologist was in a small, poorly funded healthcare facility and my breast specialist was 40 miles south instead of in that town’s system, she gave me my tests physically and told me I legally could not look at them and to give them to the specialist.
The breast specialist told me that was wrong. I could look at my tests and the radiologist should have been more open with me. The tumor had almost doubled in size from the first time it had been recorded via ultrasound(?) to the mammogram. She let me know that there was a good chance it was cancer and fast-spreading. When she told me her company charges 1,100 upfront for a biopsy, I told her I’d be back in six months, and her response was, “If it’s cancer, you might not have six months.” That’s how bad it looked (I was also malnourished at the time which caused other symptoms). She then offered to pay for a lot of it so I had to pay only ~400 of it she was so sure it was cancer. I came back the next day.
I was scared. I thought I was going to be fighting an uphill battle with cancer. But I was a hell of a lot less scared when the doctor was honest to me. None of the doctors I had seen up to that point had let me know how serious it was. Because no news is good news, there was two months between my first visit with an OBGYN and finally seeing the breast specialist. Had my doctors been honest with me, I’d have not rescheduled my appointments around work. That two months could have been the difference between life and death. When my breast specialist lowered the price so I could afford it (well a family member paid for it), I got in the next day to have the biopsy even though I had a final presentation at school.
To this day, I am angry. Yes, I would have freaked out if I saw how bad it was. But I also wouldn’t have rescheduled my appointments. Sure, it turned out to be benign, but both my then Breast Specialist (who retired) and my current one agreed that it looked like textbook cancer and it looked bad. I now only see doctors that publish my labs WITH EXPLANATIONS for me to see.
> told me I legally could not look at them
Was this in the US, after 2000?? If so, that’s an outrage! Completely false. Whether it was a lie or a seriously misinformed provider, that’s a significant failure of professionalism.
I’m glad you don’t have breast cancer, but boy … and I know what you mean about being exposed to bad news. The truth may scare you, but that scare is sometimes what enables you to do what you need to do. In this case that paternal action, even if it was well-meaning, led to you being disempowered and thus making an uninformed decision.
Keep fighting for what’s right. Thanks for your contribution.
So, what I hear is that the clinicians themselves have trouble understanding all the implications of their images and reports. They need to work as a team to help the patients. Once they understand their limitations, they probably would be able to understand that the patient – another interested party – should be included.
I do not deny the need of the patient to have their images, but this would make things better for maybe 1% of patients that are able to engage meaningfully with the images. We still have a lot of other patients to help and a whole lot of clinicians better work in teams.
We’re still just nibbling at the edge of the healthcare system.
I run the “National Organization for Medical Malpractice Victims”_ Facebook group, and we advocate for black box recording devices, because patients find accurate medical records so difficult to obtain in many cases. It’s time to share information and technology with patients. It’s a new century! If we don’t share with patients, we will lose their trust.
I agree that part of the problem is that practitioners don’t always get the full story or communicate with each other when it would be most helpful. However, I disagree with your assessment that getting data into the hands of patients will only help the “1% of patients who are able to engage with the information”. All patients have a need to have control over their information, even if they don’t understand all of it. As in my story above, if a patient sees multiple doctors, or moves to a new location and thus needs a new doctor, the only really effective way to get all important information into the hands of the new doctor is to bring it with you. You can sign release forms all you want, but there’s no guarantee that the back office will successfully acquire all of your history, especially in a timely manner. So yes, only some patients will be able to use the data as you suggest, to help the doctor SEE the problem, but ALL patients can use the data to make sure doctors have access to it.
Dave, a brief story. 6 yr old daughter had a swollen finger for 2 days that was still sensitive to touch- so we went to pediatrician walk in hours on a Friday. They sent us to local X-ray facility. X-ray tech wasn’t sure but thought it was broken, I got CD. I drove to my husband’s office (his computer had CD drive). He opened images and I sent cell phone text with image to my sister who is ER Doctor in another state. She said we’d need pediatric ortho. I drove kid to Boston pediatric ortho for their walk in hours (called for appt on the way). Was seen, casted and was driving home in Friday lunch time traffic when pediatrician called back and said “X-ray was reviewed and there’s a break, you’ll need to make an appointment with pediatric ortho on Monday” I think they fell out of their chair when I said “oh we are all set, we have already been seen, gotten casted and are on our way home” Now I know to skip the step of stopping by the pediatrician’s office – and we just go to pediatric ortho walk in hours (further drive but faster results). Thanks for asking!!!
HA! Good for you!
As a kidney cancer patient advocate, I have read endless stories of the patient finding out that an earlier CT scan showed a primary tumor on the kidney found when the patient was thought to have gall bladder disease or a broken rib. When the anticipated problem was not found, the doctor did not read the rest of the report in which there was an area ‘suspicious for metastasis” or ‘Mass found in kidney”. After being treated for 8 months for ‘tiny, scabbed-over stomach ulcer’, and then being diagnosed with a large kidney tumor, I finally got the pathology report. “No frank ulcer”, and “no H.pylori”. Also got the admitting ER doctor’s recommendations which noted that I should be seen by a hematologist or rheumatologist–but was assigned by the hospital to be seen by a gastroenterologist. Patients NEED every bit of data and interpretation of that day as soon as it is produced. I take the stance that if I as a patient do not have access to my data, than I assume that the doctor also cannot have such access, so I am being treated without the available information.
PS. The magic question, “What else could it be?” is now joined by, “What information did you use to come to that diagnosis?” (Of course, I will ask/demand the data.) Essentially, a request for a rationale for diagnosis.
Superb tutorial, Peggy!
For those who don’t know, Peggy is (or at least was) involved with the Society to Improve Diagnosis in Medicine, and you can see why.
Dave and All SPMrs, I am indeed still involved with the Soc. to Improve Diagnosis in Medicine, with an upcoming November conference in New Orleans, where Helen Haskell and I will open the conference with a Patient Summit. Not just ‘for’ patients, but led and produced by patients. Open to patients who have a concern for these issues. Similarly, Helen and I and other SIDM people gave a day long immersion workshop at the IHI/NPSF (patient safety) conference. After all, what is inherently less safe than a wrong diagnosis, missed diagnosis and the wrong or delayed treatment. A far bigger issue than the doctor not washing his hands–or is it? And who thought a patient had to worry about getting sick from his providers or from central line infections or falling out of his bed or….
I am in the midst of a similar kind of situation. I have a growing pre-laryngeal nodule. Nobody was taking it seriously until I stomped my feet and pouted. Got in to see an ENT onc, who did a FNA and said it’s cancerous. OOOOOokkkkkkkkk…….
Here’s the kicker. They said they presumed it was metastatic thyroid cancer, although FNA of the thyroid was clean. I asked for further info, so they looked back at CT scans of my neck from 2-3 years ago.
“Oh, that nodule has been there for awhile,” they said then.
When the doctor showed me the CT scan images once, after that I could pick it out every time we’d scroll through.
How does a radiologist not even note an anomaly like that, in his/her report — even if that particular anomaly was not the presenting cause for the CT scan in the first place?
Thread: https://twitter.com/GilmerHealthLaw/status/1004050622675496961
I once looked at an x-ray of my hand in the ER. The doctor had been trying to dig out what he thought was a tooth fragment. What he saw on the x-ray was on the first joint of the finger. Where he was digging was on the second joint. If we’d both looked at the x-ray at the beginning, I could have saved us both time and me some expense and pain.
Sorry for the delay in responding, Liz. If I’m reading this correctly, it seems a little bit appalling that it would be possible to look at an x-ray and then cut into the wrong joint. I know I haven’t seen the x-ray nor do I have any training on such things, but it sure does seem (as you say) that it makes sense to have a second set of eyes!
Curiosity – did he say anything like “Holy crap – sorry!!”?
I found a rare disorder on my CT images that were totally missed on the radiology report! Double Birds Beak Sign in thoracic spine! It was so obvious that it wasn’t normal and bone spurs were protruding into my esophagus!
An audience member from this event wrote to ask if there are websites where you can upload an image and get informed comments. Facebook thread is here. Discussion is mostly “Watch out”, which I of course agree with – OTOH, all the examples here make me feel just as strongly that nobody should be discouraged from understanding as much as they can, and asking questions.
The FB thread: https://www.facebook.com/epatientdave/posts/10216040327898818